Hopper L, Shanahan M, Vines A, Daniels J, Bharathi Z, Hussey J. Fathers and child health behaviors: assessing father engagement, early childhood diet, and screen time in a national sample of US children. HPHR. 2021;36.
DOI:10.54111/0001/JJ5
The impact of father-child engagement on early childhood obesity risk has not been thoroughly investigated. In response to this gap, relationships between father-child engagement at age 2 years and multiple obesity risk factors at preschool were estimated in 4,500 families belonging to the Early Childhood Longitudinal Study – Birth Cohort (ECLS-B). Early childhood obesity risk factors were prevalent in this US national sample, including weekly fast-food consumption (76%), excess juice (73%) and sugar-sweetened beverage (31%) use, and screen time above national recommendations (26%). Multivariable regression models revealed a mix of positive, negative, and null impacts of father engagement on pre-school obesity risk factors. Father engagement through both caregiving and play decreased juice consumption (Adjusted Relative Risk [aRR] = 0.87; 95% CI: 0.83, 0.98 and aRR = 0.82; 95% CI: 0.79, 0.91, respectively). On the other hand, father engagement in caregiving increased the risk of excess screen time (aRR = 1.06; 95% CI: 1.02, 1.12) and father engagement in play predicted lower fresh fruit consumption (aRR = 1.06; 95% CI: 1.01, 1.23). Finally, engagement through father-child shared breakfast decreased the risk of excess screen time (aRR = 0.95; 95% CI: 0.93, 0.98). These findings suggest that father-child engagement has both positive and negative impacts on early childhood obesity risk factors. The findings from this study, like prior ones, also reflect how underdeveloped this line of research is and how strong the need is for additional works that will provide us with actionable evidence on which to base policy.
Obesity is an urgent threat to the immediate and long-term health and well-being of children.1-3 The latest data from State of Obesity show that the prevalence of the disease has continued to trend upward since the early 1970s.4 The national obesity rate among youth ages 2 to 19 years is 18.5%, compared to approximately 13% just two decades ago.5 If these trends persist, it is estimated that by the year 2030 86% of the US adult population will be overweight or obese.6 Overweight/obesity during childhood has immediate health impacts ranging from increased breathing problems to increased social problems such as bullying and lower self-esteem.7-8 In addition to the immediate consequences of developing obesity in early childhood, these children are more likely to become adults with obesity and suffer from more severe adverse outcomes in adulthood.9-10 Obesity, which accounts for nearly 300,000 deaths each year, is the second leading cause of preventable death among US adults.11 The consistent upward trend and alarming projections, along with the lifelong health implications, highlight the need to position understanding the etiology of early childhood overweight/obesity as an urgent public health priority.
Diet and physical activity are two of the strongest behavioral predictors of obesity.12 Children require healthy diets and regular activity to support optimal cognitive, emotional, and physical growth and development. Currently, children do not meet national diet and physical activity recommendations. 13-16 The Centers for Disease Control and Prevention (CDC) notes that while children are eating more fruit than previously, vegetable consumption remains low, and both still fall below the national dietary guidelines.17 In addition, only one in three children meet physical activity recommendations and screen time has more than doubled for young children since 1997.18-19
Parents have an early and important influence on childhood obesity risk. In early childhood, when learning is occurring so rapidly, eating preferences are also developing.20 The increasingly recognized role that families play has boosted research on parenting and other family factors that may impact child obesity.21-22 Pearson, Biddle, and Gorely conducted a systematic literature review to evaluate associations between family environment and child fruit and vegetable consumption and concluded that children generally mirror the eating behaviors of their parents.23 More recent findings suggest that both mothers’ and fathers’ engagement of children in meal preparation was associated with lower child nutrition risk.24-25 Further, fathers’ modeling of healthy behaviors was associated with lower nutrition risk.24-25
However, within the parent-focused literature on childhood obesity, relatively little evidence exists on the specific influence of fathers. A systematic literature review examining the influence of parenting on childhood obesity between 2009-2015 found that only 10% of over 650 studies presented results for fathers.26 This review also concluded that studies including fathers were less likely to focus on diet and young children (aged < 5 years). Existing studies on fathers were mostly cross-sectional and relied heavily on proxy reports of father engagement from the mother.27-30
A noteworthy exception is the work of Guerrero and colleagues, which leveraged longitudinal data from the Early Childhood Longitudinal Study – Birth (ECLS-B) cohort and direct reports from fathers on their engagement with their children.31 These authors estimated the relationship between six measures of father-child engagement at age 2 years and five obesity-related health behaviors at preschool (age 4 years). Specifically, the authors found that more frequent father-child meals outside the home were associated with excessive sugar-sweetened beverage and fast-food consumption. Additionally, more frequent father-child breakfasts increased the risk of child overweight/obesity status. Sharing breakfast with fathers was found to be modestly protective against sugar-sweetened beverage consumption. 31
Building on the work of Guerrero and colleagues, this study will also draw on the ECLS-B to examine how father engagement at age 2 years influences obesity-related health behaviors at preschool. Our conceptualization and measurement of father-child engagement offers an important extension of their work. While Guerrero et al. and others have modeled individual indicators of father-child engagement, we will apply exploratory factor analysis (EFA) to identify multiple indicators derived latent constructs of father engagement. 21,31 This approach will make better use of the multiple and correlated indicators of father-child engagement measured in ECLS-B.
Our study utilizes mother, father, and child data from the Early Childhood Longitudinal Study – Birth Cohort (ECLS-B). ECLS-B is the first of three longitudinal studies, conducted by the National Center for Education Statistics (NCES), examining child development as well as early school experiences.28 The cohort is a nationally representative probability sample of approximately 14,000 US children born in the year 2001 and followed annually through kindergarten entry. The sample was captured through a complex multistage survey design, including oversampling children who met certain criteria (twins, born low birth weight, American Indians, and Asian/Pacific Islanders). More information on ECLS-B is available in the literature.32
Children were included in the analytic sample if they 1) had 2-year resident father self-administered questionnaire data; 2) had the same resident father reported by the biological mother across data collections; and 3) had complete parent self-administered questionnaire data on outcomes of interest at the preschool survey collection. The final analytical sample included approximately 4,500 child-mother-father triads. The sample size is rounded to the nearest 50 to comply with ECLS-B’s restricted data requirements.
Obesity-related health behaviors (preschool). We examined six obesity-related health behaviors reported by the mother at the preschool (age 4 years) parent self-administered questionnaire. Mothers provided detailed information on child eating habits and the number of hours their child watched television per day. These variables were coded as inadequate or excessive if they do not meet the American Academy of Pediatrics (AAP) or the US Department of Health and Human Services (DHHS) and US Department of Agriculture (USDA) guidelines for child nutrition and screen time.14,33 The five diet measures were excessive fast-food consumption, inadequate fruit consumption, inadequate vegetable consumption, excessive sugar-sweetened beverage (SSB) consumption, and excessive juice consumption. Mothers reported these behaviors based on the week before the survey was completed. Frequency response categories were collapsed into binary variables distinguishing between behaviors consistent with (coded = 0) and not consistent with (coded = 1) these recommendations. Following prior ECLS-B work, fast-food consumption was considered excessive if the primary caregiver reported the child ate fast-food at least once in the past seven days.31 SSB consumption was considered excessive if the primary caregiver reported the child had a SSB at least 4 times or more in the past week. Juice consumption was considered excessive (and unhealthy) if the primary caregiver reported the child had 100% juice beverages at least 4 times or more in the past week. While juice may be considered a healthier alternative than SSBs, it is often overconsumed by children and contributes to increased sugar intake.34 Fruit and vegetable consumption was inadequate if the primary caregiver reported the child did not have a fruit or vegetable serving at least once per day in the last week. Screen time was excessive if the primary caregiver reported the focal child averaged more than two hours of screen time per day in the past week.
Resident father engagement. The level of resident father engagement at age 2 years was measured with two-factor scores representing the frequency of caregiving and play activities, respectively. Resident fathers were asked thirteen questions about their level of involvement with child activities in the past month, with six response options ranging from “more than once a day” to “not at all.” The thirteen specific activities assessed were: 1.) play chasing games with your child; 2.) prepare meals for your child; 3.) change your child’s diapers or help your child use the toilet; 4.) take your child for a ride on your shoulders or back; 5.) play with games or toys indoors with your child; 6.) help your child to bed; 7) give your child a bath; 8) take your child outside for a walk or to play in the yard, a park, or a playground; 9.) help your child get dressed; 10.) go to a restaurant or out to eat with your child; 11.) assist your child with eating; 12.) help your child brush his or her teeth; 13.) take him or her with you to a religious service or religious event. Additionally, fathers were asked how many days “in a typical week” they eat breakfast with the child (range: 0-7).
For the study, exploratory factor analysis, a widely utilized statistical technique in the social sciences for variable reduction, was conducted using the 2 year resident father self-administered questionnaire.35-36 In addition to potentially identifying one or more latent father engagement constructs, EFA can be a more efficient way to summarize multiple related items into a smaller number of factor scores (i.e., data reduction), and provides additional information on how well individual items explain an underlying factor.37 In order to take the most comprehensive approach to capture father engagement, all of the items were included in a factor analysis – of which twelve were retained – to create two father engagement latent variables, caregiving, and play.
Factor 1, “Caregiving”, included 7 of the original thirteen father engagement items. The amount of time fathers reported changing diapers, dressing the child, washing the child, preparing food, putting the child to sleep, brushing the child’s teeth, and assisting with eating loaded onto this “Caregiving” factor. Factor 2, “Play,” included five of the original thirteen father engagement items. The amount of time fathers reported allowing the child to ride on shoulders, playing chasing games, playing indoor games, playing outside, and eating out with the child, loaded onto this “Play” factor. Cronbach’s alphas for the 7 caregiving items and 5 play items were 0.82 and 0.65, respectively. The religious services item was removed from further analysis as it failed to load onto the two father engagement factors. Fathers were asked to report the number of days they ate breakfast with their child in the past week.
Covariates. Also included are additional variables identified by theory and prior research as potentially confounding the association between father engagement and obesity-related health behaviors in early childhood. Child variables were reported by the mother and included sex, prematurity status, and overall health status. Father variables included education level, self-reported health status, race/ethnicity, and current age. Maternal variables were included to capture mother engagement and included mother’s education level, self-reported health status, and the amount of time spent preparing food and engaged in play activities. Last, household income, which is likely associated with father engagement and obesity-related health behaviors, was also included as a potential confounder.
All analyses were completed using SAS 9.4. Statistical analysis proceeded in three steps. First, descriptive statistics (weighted for the sampling design) were generated and reviewed for all study variables. Next, the crude association between each independent variable and each of the six dependent variables was estimated in a series of binary logistic regression models. All independent variables, including potential confounders, were tested for collinearity before being included in the regression models for each outcome. Next, we generated adjusted estimates of the relationship between father engagement and each of the six obesity-related health behaviors. The father-child shared breakfast question was modeled as a separate indicator of father engagement because it was structured and scaled differently from the 13 items evaluated in the EFA. Each of these three father engagement variables were modeled as continuous variables in subsequent regression models. This EFA approach differs from most of the previous research that only investigated a limited number of specific father engagement questions. Sample weights, which adjusted for the complex sample design and nonresponse to the first three rounds of parent interview data, were applied to all our statistical analyses to obtain nationally representative estimates.28 To evaluate the functional form of the association between the two father engagement factor scores and child overweight/obesity, these continuous variables were also modeled as categorical (quintile-based) measures.
This study was reviewed and approved by the University of North Carolina at Chapel Hill’s Institutional Review Board (IRB) within the Office of Human Research Ethics. The study was also reviewed and approved by the University of North Carolina at Charlotte’s Office of Research & Economic Development.
The frequency of father engagement varied by type of activity performed with their child. On the one hand, over two-thirds of fathers reported helping their child to bed and playing indoors daily. However, only half of the fathers reported the following activities: preparing meals with the child (versus 83% of mothers), assisting their child with eating, playing chasing games, and helping their child get dressed at least once per day. In addition, only one-third reported frequently playing outside (versus 44% of mothers), allowing the child to ride on their shoulders, bathing their child, and helping to brush teeth. Fathers reported eating breakfast with the child around three days out of the week on average.
The five diet outcomes revealed a mix of relatively adequate and excessive behaviors (Table 1). On the positive side, most preschool participants consumed fruit (72.1%) and vegetables (67.3%) daily. On the negative side, 75.9% of children ate fast-food at least once per week and 31.0% consumed SSBs at least four times per week. 72.5% of children drank 100% juice at least 4 times per week. Screen time exposure was also remarkably high at preschool (age 4 years), with one in four (25.6%) exceeding the AAP recommended maximum of two hours per day.38
Table 1. Child and Parent Descriptive Statistics, ECLS-B Preschool (N ~ 4500a)
N | [Weighted % or Mean (SD)] | |
Child Demographics | ||
Child’s assessment mean age (months) | 52.2 (4) | |
Child Sex | ||
Male | 2300 | 51.6 |
Female | 2200 | 48.4 |
Prematurity (Gestation – weeks) | ||
Full gestation (≥ 37 weeks) | 3350 | 90.0 |
Moderately Preterm 28 to <37 | 950 | 9.6 |
Extremely Preterm <28 | 100 | 0.4 |
Birth Weight | ||
Normal | 3450 | 93.9 |
Low Birthweight | 1050 | 6.1 |
Child Health Status | ||
Excellent/Very Good/Good | 4400 | 98.3 |
Fair/Poor | 100 | 1.7 |
Child Health Behaviorsa | ||
Fast-food Consumption | ||
At least once a week | 3300 | 75.9 |
Less than once a week | 1200 | 24.1 |
Child Fruit Intake | ||
At least once per day | 3250 | 72.1 |
Less than once per day | 1250 | 27.9 |
Child Vegetable Intake | ||
At least once per day | 3050 | 67.3 |
Less than once per day | 1450 | 32.8 |
100% Juice Intake | ||
At least 4 times per week | 3300 | 72.5 |
Less than 4 times per week | 1200 | 27.5 |
Child Sugar-Sweetened Beverage Consumption | ||
At least 4 times per week | 1350 | 31.0 |
Less than 4 times per week | 3150 | 69.0 |
Child Screen Time (Hours per Day) | ||
More than 2 | 1100 | 25.6 |
Less than or equal to 2 | 3250 | 74.4 |
Household Income | ||
25,000 or Less | 650 | 16.1 |
25,001-50,000 | 1150 | 27.0 |
50,001-100,000 | 1700 | 36.2 |
100,001 or More | 1000 | 20.8 |
Father’s race/ethnicity | ||
White, non-Hispanic | 2650 | 68.3 |
Black, non-Hispanic | 300 | 5.6 |
Hispanic | 700 | 21.0 |
Asian | 650 | 3.4 |
Other, non-Hispanic | 200 | 1.8 |
Father Education Level | ||
Less than HS | 550 | 14.0 |
HS Diploma/Equivalent | 950 | 22.1 |
Some College/Associate | 1250 | 29.3 |
Bachelor’s degree or higher | 1750 | 34.6 |
Father’s age in years | 33.4 (6.5) | |
Father’s Employment Status | ||
Working | 4200 | 94.0 |
Not Working | 300 | 6.0 |
Father’s Health | ||
Excellent/Very Good/Good | 4100 | 94.3 |
Fair/Poor | 250 | 5.7 |
a Data are weighted to be representative of all children born in the US in 2001, clustered, multi-stage sampling design and oversamples. | ||
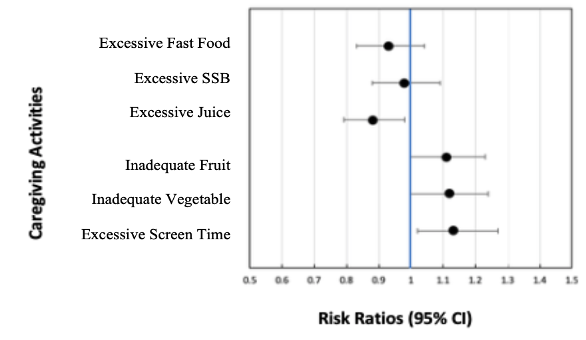
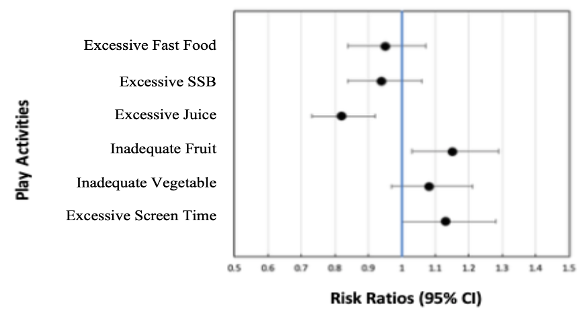
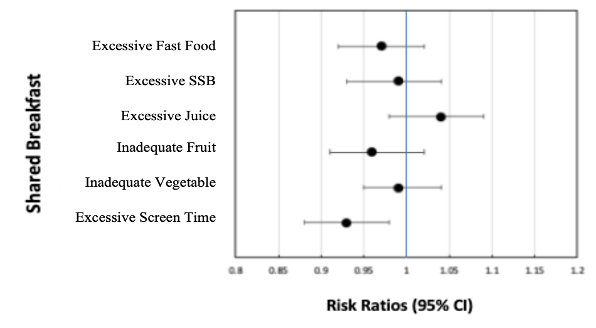
Seven of 18 total unadjusted associations between the three father engagement measures and the six obesity-related health behaviors (Table 2) were statistically significant. Increasing father engagement via caregiving lowered the risk of excessive fast-food consumption (RR = 0.92; 95% confidence interval [CI]: 0.86, 0.99) and excessive juice consumption (RR = 0.96; 95% CI: 0.95, 0.99). Increasing father engagement via caregiving increased the risk of excess screen time (RR = 1.11; 95% CI: 1.06, 1.18). Increasing father engagement via play lowered the risk of excessive SSB consumption (RR = 0.93; 95% CI: 0.87, 0.99); excessive juice consumption (RR = 0.94; 95% CI: 0.92, 0.96); and inadequate (not meeting the recommendations of one daily serving) fruit consumption (RR = 0.96; 95% CI: 0.94, 0.98). Finally, father-child shared breakfast lowered the risk of excess screen time (RR = 0.95; 95% CI: 0.92, 0.98). Increasing father engagement via caregiving was not significantly associated with the other four obesity-related health behaviors. A summary of these analyses is provided in table 2 below and illustrated in the forest plots provided in Figure 1.
Table 2. Bivariate associations between types of father engagement with early childhood obesity-related health behaviors: ECLS-B 2 year & Preschool N ~ 4200a,b
Characteristic | Excessive Fast-food Consumption | Excessive Sugar-Sweetened Beverage Consumption | Excessive Juice Consumption | |||
Father Engagement | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) |
|
| |||||
Caregiving | 0.92 | (0.86, 0.99) | 1.01 | (0.96, 1.06) | 0.96 | (0.95, 0.99) |
Play | 0.97 | (0.95, 1.05) | 0.93 | (0.87, 0.99) | 0.94 | (0.92, 0.96) |
Father-child shared breakfastd | 0.98 | (0.98, 1.13) | 0.98 | (0.95, 1.01) | 1.01 | (1.00, 1.02) |
| Inadequate Fruit Consumption | Inadequate Vegetable Consumption | Excessive Screen Timec
| |||
| RR | (95% CI) | RR | (95% CI) | RR | (95% CI) |
Father Engagement |
| |||||
Caregiving | 0.98 | (0.96, 1.00) | 0.97 | (0.95, 1.00) | 1.11 | (1.06, 1.18) |
Play | 0.96 | (0.94, 0.98) | 0.98 | (0.95, 1.00) | 1.05 | (0.99, 1.13) |
Father-child shared breakfastd | 1.01 | (1.00, 1.02) | 1.00 | (0.98, 1.01) | 0.95 | (0.92, 0.98) |
a Data are weighted for nonresponse to be representative of all children born in the US in 2001. The sample size is rounded to the nearest 50 to comply with ECLS-B’s restricted data requirements. b Abbreviations: CI, confidence interval. c Recommended Screen Time is less than 2 hours per day (N ~ 4,100). d Breakfast N ~ 3,900. *Note: The items of the ECLS-B questionnaires have undergone validation research and are useful for generating population estimates on numerous developmental, health, and educational indicators. Bold text show statistically significant association at alpha 0.05. | ||||||
In the multivariable analysis, associations between the three measures of father engagement and the six obesity-related health behaviors were adjusted for potential confounders. Of the seven significant bivariate associations, five remained statistically significant after adjusting for the full set of potential confounders. None of the three father engagement variables were found to be associated with excessive fast-food consumption, excessive sugar-sweetened beverage consumption, or inadequate vegetable consumption (Table 3). However, increasing father engagement via caregiving activities (aRR=0.87; 95% CI: 0.83, 0.98) as well as play activities (aRR=0.82; 95% CI: 0.79, 0.91) were associated with a lower risk of excessive juice consumption, adjusting for father, maternal, child, and household characteristics (Table 3). Father engagement via caregiving was also associated with an increased risk of excessive (greater than 2 hours) screen time (aRR=1.06; 95% CI: 1.02, 1.12). Father engagement via play was associated with an increased risk of inadequate fruit consumption (aRR=1.06; 95% CI: 1.01, 1.23), adjusting for potential confounders (Table 4). Finally, father-child shared breakfast was associated with a lower risk of excessive screen time per day (aRR=0.95; 95% CI: 0.93, 0.98) (Table 4).
Table 3. Multivariable associations between types of father engagement with early childhood obesity-related health behaviors: ECLS-B 2 year & Preschool N ~ 3,600a,b
Characteristic
| Excessive Fast-food Consumption | Excessive Sugar-Sweetened Beverage Consumption | Excessive Juice Consumption | |||
| RR | (95% CI) | RR | (95% CI) | RR | (95% CI) |
Father Engagement |
|
|
| |||
Caregiving | 0.98 | (0.97, 1.00) | 0.98 | (0.94, 1.02) | 0.87 | (0.83, 0.98) |
Play | 0.98 | (0.97, 1.01) | 0.95 | (0.90, 1.12) | 0.82 | (0.79, 0.91) |
Father-child shared breakfastd | 0.99 | (0.98, 1.00) | 0.99 | (0.97, 1.01) | 1.01 | (1.00, 1.02) |
a Data are weighted for nonresponse to be representative of all children born in the US in 2001. The sample size is rounded to the nearest 50 to comply with ECLS-B’s restricted data requirements. b Abbreviations: CI, confidence interval. c Breakfast N ~ 3,900. *Note: The items of the ECLS-B questionnaires have undergone validation research and are useful for generating population estimates on numerous developmental, health, and educational indicators. Bold text show statistically significant association at alpha 0.05
Results have been adjusted for: child birthweight, child sex, gestation, father race/ethnicity, father age, father education, father/mother/child health status, household income, mother prepared meals, and play with mother. | ||||||
Table 4. Multivariable associations between types of father engagement with early childhood obesity-related health behaviors: ECLS-B 2 year & Preschool N ~ 3,600a,b
Characteristic | Inadequate Fruit Consumption | Inadequate Vegetable Consumption | Excessive Screen Timec | |||
| RR | (95% CI) | RR | (95% CI) | RR | (95% CI) |
Father Engagement |
|
|
| |||
Caregiving | 0.97 | (0.95, 1.22) | 0.97 | (0.95, 1.13) | 1.06 | (1.02, 1.12) |
Play | 1.06 | (1.01, 1.23) | 0.98 | (0.95, 1.00) | 1.06 | (1.00, 1.12) |
Father-child shared breakfastc | 1.01 | (1.00, 1.02) | 1.00 | (0.99, 1.01) | 0.95 | (0.93, 0.98) |
a Data are weighted for nonresponse to be representative of all children born in the US in 2001. The sample size is rounded to the nearest 50 to comply with ECLS-B’s restricted data requirements. b Abbreviations: CI, confidence interval. c Breakfast N ~ 3,900. *Note: The items of the ECLS-B questionnaires have undergone validation research and are useful for generating population estimates on numerous developmental, health, and educational indicators. Bold text show statistically significant association at alpha 0.05
Results have been adjusted for: child birthweight, child sex, gestation, father race/ethnicity, father age, father education, father/mother/child health status, household income, mother prepared meals, and play with mother. | ||||||
Figure 1. Summary Forest Plots of Relative Risks between types of father engagement with early childhood obesity-related health behaviors, adjusted for child parent socio-demographics N ~ 3,600
This work builds upon a limited number of studies examining how father engagement impacts early childhood obesity-related health behaviors. In a nationally representative sample, father engagement was protective against three obesity-related health behaviors, predicted higher risk for two, and was not associated with the majority of those examined. Specifically, father engagement via both caregiving and play was protective with respect to excess juice consumption and the frequency of father-child shared breakfasts was protective against excessive screen time. On the other hand, father engagement via play reduced fruit consumption and father engagement via caregiving increased the risk of excessive screen time.
Findings from this work are mostly consistent with the two previous ECLS-studies on father engagement and obesity risk.21,31 First, like this current work, both previous studies did not find support for most of their predicted associations. Of the thirty total associations (six father engagement indicators x five obesity risk outcomes) that Guerrero et al. tested, only four were significant. 31 The current study along with Guerrero’s work both found shared breakfast to be associated with various obesity-related health behaviors. Similarly, only two of the twenty associations between change in father engagement (physical caregiving and taking their child outside) and change in obesity risk estimated by Wong et al. were significant. 21 These were the same father engagement behaviors captured by the caregiving and play constructs in the current study that were found to be associated with obesity-related health behaviors. Second, like the other two ECLS-B studies, in the small subset of significant associations, father engagement had a mix of positive and negative impacts on childhood obesity risk. 21,31 These similarities were found despite differences in measurement and analysis approaches. This “duality” of father impacts on childhood obesity risk has also been reported in other (i.e., non-ECLS) studies.39
The small and mostly non-significant associations in this study are also consistent with findings from parent-focused childhood obesity interventions. A recent meta-analysis of 76 early childhood interventions involving parents reported a small overall effect size (d = .08) and no effect at all for follow-up periods longer than 3 months.40 Perhaps the 24-month interval between ECLS-B’s measurement of father engagement (Age 2) and assessment of obesity risk behaviors (Age 4) was too long to detect any father effects that may truly exist. Future observational studies might follow the approach of childhood obesity randomized control trials and schedule follow-up periods of 12 months or less.41
Finally, future studies should measure and analyze a more comprehensive set of variables related to the child’s family and community environment. While engagement (i.e., direct father-child interaction) has received more research attention than Lamb et al.’s other two father involvement components—accessibility and responsibility—this is because it is easier to measure rather than because it is most important for child outcomes.39,42 Future research should study accessibility (i.e., father’s presence or availability to the child) and responsibility (i.e., the extent to which a father arranges for resources to be available to the child) to examine whether these dimensions of father involvement impact early childhood obesity risk.43 In addition, there is some evidence that a father’s overall parenting style (i.e., authoritative; permissive; etc.) impacts their child’s preschool obesity risk.44 Future studies might also assess parenting style as a possible modifier of the father engagement-child obesity risk association.
The most important limitations of this study relate to measurement. The challenges of measuring father engagement and obesity risk behaviors are well known.38,45 A limitation that the ECLS-B father engagement questions share with many other surveys is that they only ask about frequency (quantity) when there is evidence that engagement quality also matters.46 Also, the small number of child diet questions in ECLS-B do not cover all diet-related obesity risks. Standard food frequency questions used in large surveys typically ask about 100-150 foods eaten over a six- or twelve-month period (Shim, Oh, & Kim, 2014).45 Additionally, when compared to nutrition biomarkers, food frequency self-reports result in significantly weaker associations between diet and chronic disease risk.47 Lastly, both the father engagement and parent reports of child diet and screen time were likely affected by social desirability and recall bias, which could also weaken observed associations.48
On the other hand, the rare availability of both father engagement and early childhood obesity risk variables was an important strength of this data source. The multiple items on father engagement provided a unique opportunity to follow theoretical recommendations and examine father engagement as a multi-dimensional construct.49-50 This is the first known study in the early childhood obesity literature to identify and estimate associations with two latent measures of father engagement. Data strengths also include the longitudinal design, in which father engagement was measured prior to obesity-risk, and the nationally representative sample of U.S. children estimates born in 2001 and living with resident fathers. Lastly, resident fathers were included in the data collection, providing a unique opportunity to study their engagement and behaviors. Many studies that focus on fathers and child health outcomes use cross-sectional data and collect father information from the mothers.29 While it is valuable to obtain father engagement reports directly from fathers, maternal reports tend to show lower frequency of father engagement and objective measurement by trained observers has the highest predictive validity among all of these sources.49,51-52
In conclusion, understanding the etiology and reducing the prevalence of early childhood obesity is a public health priority and necessary for those who specialize in obesity prevention.53 The family environment, parental influence is a major influence on early childhood obesity risk.54-55 However, within the parent-focused literature on childhood obesity, relatively little evidence exists on the specific influence of fathers. The reality is that resident fathers have never been more involved in parenting, and the potential for resident fathers to impact early childhood obesity risk is abundant.56 This study, like prior ones, suggests that fathers can increase or decrease childhood obesity risk. The mixed findings from this study, like prior ones, also reflect how underdeveloped this line of research is and how strong the need is for additional works that will provide us with actionable evidence on which to base policy.
Dr. Lorenzo N. Hopper is an Assistant Professor in the Department of Public Health Sciences and serves as Director of the Master of Public Health program. Dr. Hopper’s areas of research interest include fatherhood, men’s health, understanding and address health disparities, and the first-generation college student experience. He received his formal training at the University of North Carolina at Chapel Hill.
Dr. Shanahan is a research assistant professor in the Department of Maternal and Child Health and a research scientist at the UNC Injury Prevention Research Center. The underlying motivation for Dr. Shanahan’s research is to improve the health and developmental trajectories of children. Her research focuses on adverse events that potentially influence these trajectories and prevent children from realizing their full potential.
Dr. Vines’ research centers on understanding the underlying determinants of health disparities with interests in community-based research, chronic disease epidemiology and cancer.
Dr. Daniels’ research focuses on prenatal environmental and nutritional exposures that may impact children’s growth, neurodevelopment, and overall health. She has created a platform for studying early life exposure to brominated and organophosphate flame retardants, persistent organic pollutants, and long-chain fatty acids as they relate to children’s health in the Pregnancy, Infection & Nutrition Kids Study
Dr. Bharathi Zvara is a research assistant professor whose research interests focus on parenting, parent-child relationships, and early normative and atypical development from a biopsychosocial developmental perspective. Her research seeks to identify psychobiological and environmental mechanisms linking childhood experiences of trauma, violence, and social disadvantage to the development of children’s self-regulation, emotions, and behaviors.
Dr. Jon M. Hussey is sociologist and demographer with a primary interest in the association between social stratification and health. He is particularly concerned with the causes of racial, ethnic, and socioeconomic differentials in morbidity and mortality. Understanding how childhood exposures influence adult health disparities is a specific objective of his work.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()