Irfan A, Slimko M, Carrasco H, Eaton T. The DrPH Coalition: advancing public health practice and leadership in the 21st Century. HPHR. 2021;35.
DOI:10.54111/0001/II10
This article provides a brief background on the history of the Doctor of Public Health (DrPH) degree, draws a distinction between a DrPH (a practice-based, leadership training degree) with PhD (research-based degree), lists CEPH competencies and DrPH community training needs, and highlights the critical need for competent practitioners to lead the public health responses. Further, it also introduces the DrPH Coalition, a grassroots organization focused on advocating the systems change efforts including uplifting competently trained public health practitioners and leaders. It also introduces the HPHR-DrPH Coalition collaborative Special Edition (35).
The 1915 Welch–Rose Report (Welch-Rose Report, 1915), which set the foundations for schools of public health, reflected the tension between different preferences of the plan’s two architects: William Henry Welch favored scientific research, whereas Wickliffe Rose wanted an emphasis on public health practice. Welch’s approach won the argument at the time and the new discipline was nudged to a largely laboratory-based and research-focused educational training system — a trend that persists today. The calls for more applied, practice-based leadership training have also continued to echo. Roemer (Abel et al., 2008), a visionary of his times whose ideas continue to guide the field of public health today, was an authority on public health practice and leadership. He wrote extensively (Roemer, 1986) on the need to train public health practitioners through practice-based courses and extensive field experiences that connect theory to practice. Moreover, the Council on Education for Public Health’s (CEPH) latest criteria for Doctor of Public Health (DrPH) core courses heavily emphasizes leadership, management and governance; policy and programs; education and workforce development, and less so on mere data and analysis (CEPH, 2016). Despite these requirements, several schools continue to emphasize research in their programs that are not much different than Doctors of Philosophy (PhD).
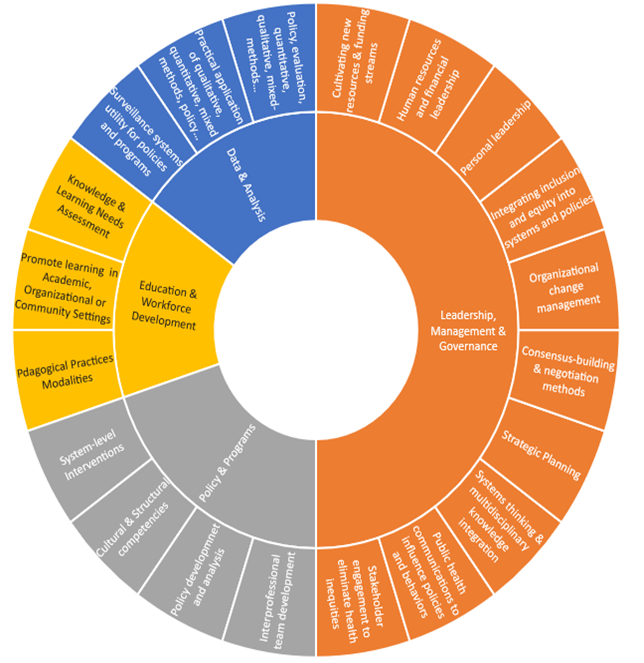
Public health practice has advanced exponentially over the last couple of decades. We now understand the appropriate skills and competence for effective public health leadership and practice. DrPH — accredited by CEPH (see figure 1 for CEPH DrPH competencies) — is the terminal, professional degree for the field of public health that is designed to train competent, effective public health leaders (ASPPH, n.d.). Universities around the United States have been offering the DrPH since the early 1900s, often with an admission requirement of holding a Doctor of Medicine at the beginning of these programs (Howe, 1918). By 1919-1920 the DrPH was recognized by the American Public Health Association as an advanced degree for physicians who wanted to practice public health, distinct from research (Abbott et al., 1921; Park et al., 2021). The DrPH was conceived as equivalent to an MD for those interested in public health, based on a similar, practice-based model that would equip its holders with strategic leadership skills and key public health practice competencies critical for effective translation of evidence, public health practice, and management. Yet, nearly a century later, the debate remains the same and an unwarranted emphasis on research-based model continue to limit the training potential of DrPH.
The SARS-CoV-2 (COVID-19) pandemic brought light to several of the gaps and challenges in public health practice and broader social infrastructure around the globe. Many factors contributed to preventable, COVID-related deaths and despair such as a continued failed federal response by the U.S. government across administrations (Mirvis, 2020), the lack of authoritative local public health mandates, the politicization of safety measures, and the lack of competent public health leaders and practitioners who are well equipped to build rapid coalitions, synthesize evidence and translate that evidence into effective public health policies: skills a DrPH degree is designed to deliver. Another harsh reality that COVID-19 has exposed is the declining public health workforce over the years when we need more, not less people in public health (Castrucci & Lupi, 2020). The dawn of a new decade with 2020 has brought a once-in-a-lifetime challenge, a global pandemic has emphasized the need for more opportunities to innovate public health practice and leadership training. Historically (IOM, 1988) and contemporarily (ASTHO, n.d.), a significant percentage of public health leadership is formed by clinicians with limited to no training in public health since medical school curriculums are not designed to train clinicians in public health. This is in part because of decades-old, ineffective laws and regulations requiring a clinical degree or license to lead public health departments without necessarily requiring formal public health training (IOM, 1988). Relics of the past, regulations that continue to misappropriate competence likely contribute to the inefficiency and leadership failures of public health systems.
Urgent need for competently trained public health leaders and practitioners has been reiterated time and time again, even before COVID-19. Especially since the field of public health relies on medically trained professionals to lead public health programs and departments, who are not trained to properly execute such functions. Since its inception, DrPH programs have struggled to successfully integrate leadership and practice into the training structures. Another challenge DrPH programs have encountered is the ability to authoritatively distinguish them from Ph.D. programs because of an emphasis on research, likely due to the academic models that reward research, publishing, and grant money over applied work focused on social impact. However, despite these challenges, DrPH programs have managed to combine evidence-based research and applied leadership skills and train well-equipped public health leaders over the years (Sherman et al., 2016). The degree has become the gold standard for public health leadership despite a slower acknowledgment by state and local health departments. In this era of chaotic global politics with old and emerging challenges from dismantling systemic racism, mental health, climate change, zoonotic diseases, it is time to go beyond narrow thinking and seize the opportunities to do even better. These challenges, concerns, and opportunities are shared by DrPH students, alumni, and prospective DrPH students.
DrPH Coalition was conceived, by starting these conversations with a large number of DrPH students through cross-school engagement, with the aim to advocate for public health practice and leadership-based education for the future public health leaders, as well as distinguishing the field of public health practice from research. In 2019, the DrPH coalition began as a grassroots, student-led effort with students from across the United States and global DrPH students supporting these efforts with shared concerns and aspirations. This novel approach with a large scale of grassroots organization and broad coalition-building by DrPH students, to forge a public health practitioner and leadership identity has not been done before. It is reflective of the contemporary needs and gaps in DrPH training and public health workforce misalignment with this doctoral degree.
Figure 2, generated through DrPH stakeholder engagement, depicts what distinguishes DrPH training from Ph.D. training. Compared with a Ph.D., a DrPH also provides effective leadership training to solve complex problems in public health practice. In addition, several DrPH program admissions require about three to five years of experience along with an MPH. This leadership training and experience prepare DrPH graduates to occupy public health leadership positions across sectors. Moreover, the DrPH training includes a heavy emphasis on leadership at the personal, organizational, and societal levels that help them be better prepared for challenging situations, such as pandemic emergency responses, where things are uncertain and ambiguous, and quick evidence-based strategies must be implemented for effective public health response.
The goal of broad coalition-building and practitioner community engagement with fellow DrPHers led to the idea to send out a call for content on pieces from DrPH students, DrPH alumni, and non-DrPH allies across public health sectors to encourage thought leadership in a way that can elevate some of the applied work that DrPHers are doing in their respective fields. Through this Special Edition and the selected articles, specifically formatted based on the editorial board’s suggested template, we aim to highlight the importance of thought leadership and applied scholarship that DrPHers produce and uplift the non-traditional approach to sharing our work that transcends original research. In this issue, you will not find original research, but rather commentaries and thought pieces that cover a wide range of public health issues including, but not limited to, the following: pandemic emergency responses, multisectoral collaboration, health disparities and health equity, implementation, public health leadership and policies, and decolonizing public health.

Our goal of advancing DrPH and applied public health remains. By convening public health practitioners, including current and future DrPH leaders, we hope to foster continued learning, networking, and dialogues that will help shape the future practice of public health to achieve a healthier world for all. DrPH Coalition remains committed to advocating on behalf of DrPH and the public health practice community through a range of programming. Together, we can dream and bring about a future rooted in global health equity through effective leadership and the application of knowledge to monumental public health challenges. We hope you enjoy this edition and be as inspired and committed to our collective movement of advancing applied public health.
The authors are grateful to the DrPH Coalition’s leadership and membership for their support in developing this issue, the DrPH Coalition’s HPHR Editorial Board for organizing, collecting, and reviewing the articles selected for this edition, as well as the DrPH Coalition members and colleagues who submitted their pieces for review.
Ans Irfan, MD, EdD, DrPH, MPH is a multidisciplinary global public health expert with over a decade of experience in advancing global health equity, both domestically and globally. He currently serves as a faculty member, researcher, and Director of the Climate & Health Equity Practice Fellowship at George Washington University. He is also a fellow with the Robert Wood Johnson Foundation Health Policy Research Scholars program. He also serves in various roles with major national and international organizations, including the American Public Health Association, Interdisciplinary Association for Population Health Science, and the United Nations Major Group for Children and Youth. Some of his recent roles include serving on the advisory board with the American Public Health Association’s Center for Climate, Health & Equity; APHA Governing Council; Policy Director with the DrPH Coalition, Inc; and the founding director of Center for Social Impact & Leadership with the DC Public Health Association. He has previously served as a fellow with the prestigious Christine Mirzayan Science Policy Fellowship at the National Academy of Sciences and the Agents of Change in Environmental Justice Fellowship.
As a critical public health scholar, he combines multiple disciplines — including global health; environmental and occupational health; health policy; migrant health; climate change; sociology; diversity, equity, and inclusion (DEI); organizational change management; program development, management, and evaluation; and implementation sciences — through a mixed-methods approach to provide innovative interdisciplinary public policy and programmatic solutions geared towards ameliorating social and health inequities. Select recent projects include: COVID-19 & Black transit workers health; farmworkers health equity; global health implications of US foreign policy; the intersection of religion and public health; traffic wardens and climate adaptation in Pakistan; evaluation of physicians’ training on climate change and health; global and occupational health equity. He can be contacted at ansirfan@gwu.edu. Twitter: @PHScientist
Michelle L. Slimko, DrPH, MPH, RD is currently the SVP of Environmental and Nutrition Research at National Dairy Council. She is a Registered Dietitian and graduated from the University of Illinois at Chicago School of Public Health DrPH Leadership Program.
Hector Carrasco MD, MPH, DrPH is the High Impact Areas program (HIA) Director at the Opioid Response Coordination Office and appointed member of the Health Equity Advisory Team at the Tennessee Department of Health. The HIA Program comprises 26 different projects being implemented by local departments of health and community-based organizations in five of the seven public health regions of the state. Previously, he worked as the Director of the Global Health Initiative at Tecnologico de Monterrey which aims to launch the first Institute of Global Health Equity in Latin America. He also served as the community programs coordinator and medical practitioner for Partners in Health, Mexico. He has several years of experience in addressing global and public health issues, including migration, primary care, and community health in Sierra Leone, India, Peru, Brazil, and Guatemala. He also worked as a public health consultant for the World Health Organization, The Global Fund to Fight AIDS, Tuberculosis, and Malaria, and the Government of Sierra Leone. Dr. Carrasco received his medical degree from the Tecnológico de Monterrey, Master in Public Health from the Johns Hopkins Bloomberg School of Public Health, and Doctor of Public Health from the Harvard T.H. Chan School of Public Health.
Tiffany M. Eaton, MPH, DrPH is currently a graduate research fellow and DrPH candidate in the Department of Community Health and Prevention at the Dornsife School of Public Health at Drexel University. Her research interests include sociocultural factors that impact obesity in Black women, food insecurity, social determinants of health, health equity, and program evaluation. Tiffany also serves as the Director of External Communications on the Executive Board of the DrPH Coalition.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()