Vest J, Cash-Goldwasser S, Bandali E, Peters Bergquist E, Holly E, Caine V, Halverson P, Embi P. Direct observation, estimates, and correlates of public mask-wearing during the COVID-19 pandemic. HPHR. 2021 29.
DOI:10.54111/0001/cc18
To estimate the prevalence of public mask-wearing in various settings through direct observation. Self-report mask-wearing is susceptible to recall bias and a desire by respondents to appear socially responsible. Direct observation of public behavior does not face such limitations and can provide differentiation between correct and incorrect mask-wearing.
Trained observers recorded public behavior between 11/01/2020-12/31/2020 at 37 sites across Marion County, Indiana. For each individual observed, data collection staff recorded a status of “masked,” “non-masked” or “partial mask.” “Masked” was defined as the presence of any cloth face covering or surgical mask that covered the mouth and nose, including the nostrils, and extended below the chin. “Non-masked” was defined as the complete absence of a face covering, a face covering that was worn only below the chin, a face covering held in a hand, a face covering hanging off an ear, or a face shield only. “Partial mask” was defined as the face covering only over the mouth or over the nose, but not both, or the nose being partially covered with the nostrils somewhat or fully visible.
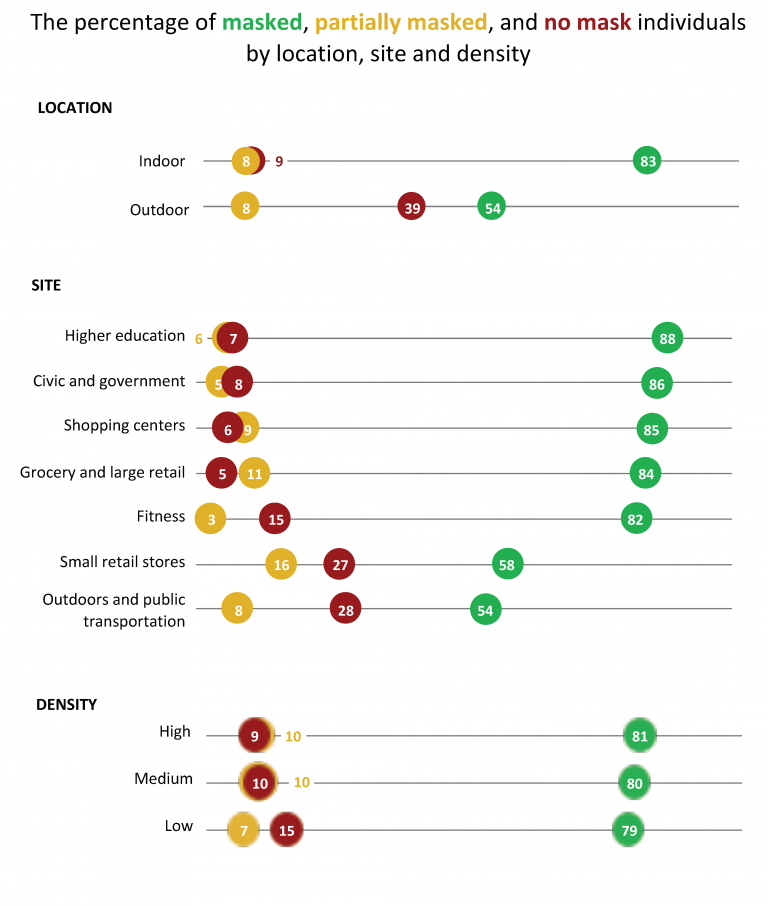
80% of adults wore face masks correctly and an additional 9% were partially masked. The prevalence of mask-wearing was lowest in outdoor spaces (54%) as well as in small retail stores (58%). Higher rates of mask usage were observed at large organizations like grocery stores and “big box” retailers (84%), shopping malls (85%), civic and government sites (86%), or higher education settings (88%). Mask-wearing was more common among females (84%) than males (76%); males had a higher percentage of partial mask-wearing.
While public health professionals and agencies encourage universal mask-wearing in public settings, observed levels may still be sufficient to reduce the spread of COVID-19.
Wearing a face mask in public is one of the most accessible and least expensive strategies to control the COVID-19 pandemic. Masks, when properly worn over the nose and mouth, can effectively filter out respiratory droplets that may contain the SARS-CoV-2 virus (Eikenberry et al., 2020). This effectiveness encompasses both medical-grade and cloth masks (Aydin et al., 2020). Outbreak investigations indicate that mask-wearing reduces the extent to which infectious people transmit the virus and provides protection for the wearer (Hendrix et al., 2020; Payne et al., 2020; Schwartz et al., 2020). Policies mandating mask-wearing have been associated with reduced risk of community-wide transmission of COVID-19 (Chernozhukov et al., 2020; Lyu & Wehby, 2020; Van Dyke et al., 2020; Wang et al., 2020).
Despite the known effectiveness of masks for reducing transmission, mask-wearing has been inconsistently adopted by the public. Self-reported mask use has varied over time, geography and demographic groups, with anywhere from 50% – 90% of adults reporting mask use in public (Bruine de Bruin et al., 2020; Hornik et al., 2020; Hutchins et al., 2020; Igielnik, 2020; IHME, 2020; Kramer, 2020; Sheehan et al., 2020). In general, the self-reported prevalence of mask-wearing in the US increased during 2020 (IHME, 2020). Although information on self-reported behaviors is valuable, these insights are subject to limitations. For one, individuals may overestimate their adherence (Igielnik, 2020; Reinhart, 2020) as survey questions reflect general behavior (e.g., “most or all of the time”(Kramer, 2020; Reinhart, 2020)). Mask-wearing may also be overreported due to social desirability bias, as the practice is commonly portrayed as appropriate, responsible, or ethical behavior by policymakers and in the media (Allan, 2020; Kamm, 2020; Kluger, 2020). Self-reported surveys also do not distinguish between correct and incorrect mask-wearing, i.e., fully covering vs. not fully covering both the mouth and nose. Still, data from observational studies, which are not subject to these limitations, are scant (Arp et al., 2020; City of Philadelphia, 2020; Haischer et al., 2020; Studio Ludo, 2020).
In light of this gap in the available data about adherence to an important public health strategy, this study aims to provide estimates of the prevalence of overall and correct/incorrect face mask usage based on direct observation of public behavior.
The prevalence of mask use was assessed through direct observation by trained staff in multiple public locations and over time in a suburban/urban metropolitan area in the United States. Data collection occurred during the period from November 1 to December 31, 2020.
All public observations occurred within Marion County, Indiana, which includes the city of Indianapolis, and is home to more than 960,000 people. In collaboration with the Marion County Public Health Department (MCPHD), the research team selected 37 observation sites that were geographically dispersed across the county to reflect socioeconomic, racial, and ethnic diversity, as well as to encompass a range of public activities, settings and communities. These locations included retail shopping and services, cultural sites, high-traffic outdoor public spaces, grocery stores, civic and community spaces, retail indoor fitness centers and university campus sites.
Data collection was limited to observable public behavior. Trained data collection staff, working in pairs or individually, counted mask-wearing behavior of all observed individuals who: 1) appeared to be over two years of age and 2) whose faces were fully visible. Data collection staff counted all individuals observed, e.g., there was no sampling strategy. At the time of the study, the U.S. Centers for Disease Control and Prevention (CDC) recommended masks for people two years of age and older (CDC, 2020). During each observation session, a given individual was counted only once and mask status was recorded at the time of observation. No identifiable data about individuals was collected, ensuring anonymity.
A uniform set of study protocols defined data collection procedures, which included a goal of observing at least 100 individuals at each site from a fixed point. Observers returned to the same set of sites regularly at varying times of day (morning 8am-12pm, afternoon 12pm-6pm, evening after 6pm) and on different days of the week (workday or weekend) over the course of the study period. Weekly team meetings were used to assess the distribution of site frequency and observer availability. The diversity of the sites necessitated some variations in observation procedure. For example, at sites with less foot traffic, the target goal of 100 individuals per session were not always observed. Additionally, some observations could not be accomplished from a fixed location within the site; in small indoor settings, for example, observers were stationed outside the site in a parking lot, collecting data on individuals as they entered or exited the site. In some outdoor settings, observers moved during data collection to be consistent with public behavior in order to be as unobtrusive as possible (e.g., walking the sidewalks of a cultural area).
Data were collected using the web-based app MaskCount (www.maskcount.com), developed by the Regenstrief Institute. The app automatically geocoded and timestamped each observation session.
For each individual observed, data collection staff recorded a status of “masked,” “non-masked” or “partial mask.” “Masked” was defined as the presence of any cloth face covering or surgical mask that covered the mouth and nose, including the nostrils, and extended below the chin (CDC, 2020). “Non-masked” was defined as the complete absence of a face covering, a face covering that was worn only below the chin, a face covering hanging off an ear, or a face shield only. “Partial mask” was defined as the face covering only over the mouth or over the nose, but not both, or the nose being partially covered with the nostrils somewhat or fully visible. Observers recorded mask status only when individuals’ faces were fully visible. The mask status was collected at the time of observation, with no exclusions (i.e., smoking, eating, or drinking). In a training dataset consisting of images of mask-wearing behavior, all 10 trainee observers exhibited very high agreement (kappa = 0.94).
Additional measures included presumed gender and session-level characteristics. Because media reports early in the pandemic suggested different behaviors by gender (e.g. Duarte, 2020), data were recorded independently for presumed males and for presumed females. If observing in pairs, each observer counted only a single gender. No other demographics were collected. Sessions were described using the time of day, day of the week, geographic location, and duration. We categorized each site as: a grocery or large retail store, shopping center (indoor), small retail store or service, civic or government site (including libraries), fitness center, higher education campus, outdoor space (park or pedestrian area) and public transportation site. We estimated the density of individuals at a given location by dividing the total number of individuals observed by the total observation time in minutes. We categorized this continuous variable in tertiles (low, medium, high).
We merged two area-level datasets based on site locations. MCPHD provided cumulative COVID-19 case counts at the census tract level, which we standardized by resident population and transformed into tertiles. Based on the most recent estimates from the Census Bureau, we calculated a Modified Townsend Index to describe socioeconomic status at the census tract.
We aggregated the individual observations from each unique site and date into single “sessions”. Session data includes the total number of observations, date/time information, frequency and percentage of each type of mask status, and linked area-level public health and social measures. We describe the total sample of sessions using means, frequencies and percentages. We report the prevalence of each type of mask use and compare characteristics within each type using one-way ANOVAs and post-hoc pairwise comparisons. Next, bivariate and fully-adjusted multivariable fractional multinomial logistic regression models described the association between characteristics and the prevalence of mask-wearing behavior using the fmlogit package in Stata (Buis, 2008). We selected correct mask-wearing as the reference category and used cluster robust standard errors that accounted for repeat sessions of the same site. We created adjusted models using a backwards elimination approach using improvements in information criterion as a guide and excluded collinear measures (e.g., indoor/outdoor with site type). To facilitate interpretation of the logit models, we expressed coefficients as marginal effects.
The total number of sessions in the sample was 368, which included a total of 25,901 individual observations. Sessions had a mean of 78.1 individuals observed (sd =57.8) and average observation time of 51.2 minutes (sd =69.9).
Nearly 80% of observed individuals wore face masks correctly (79.9; 95% confidence interval (CI) = 78.0, 81.8), 9% were partially masked (9.0; 95%CI= 8.2, 9.7) and 11% were non-masked (11.1; 95%CI=9.4, 12.9) (Table 1). The most common study sessions were at grocery and large retail sites (42%), in the afternoons (68%), and during the weekdays (74%). Men and women were observed in nearly equal proportion.
Mask behavior varied substantially by location type (Figure 1). Mask-wearing was more common in indoor (83%) than outdoor (54%) sites and at outdoor sites, non mask-wearing was much more common (39% verse 8%). The prevalence of mask-wearing was lowest at small retail stores (58%) and at outdoor spaces and on public transportation (54%). At both of these types of sites, more than one-quarter of individuals did not wear a mask. Small retail stores also had the highest proportion of partial mask-wearing (16%). For other types of sites, the prevalence of mask-wearing was generally consistent (see Appendix 1 for full details). At each location, correct mask-wearing did not differ by density (persons per observation time). However, as density increased, partial mask-wearing increased and non mask-wearing decreased.
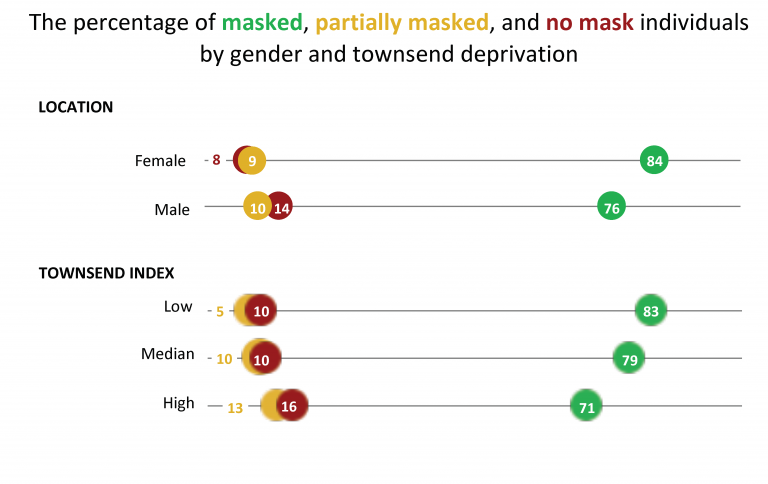
Mask-wearing was more common among females (84%) than males (76%) (Figure 2). In contrast, higher percentages of partial mask-wearing and non mask-wearing were observed among males than females. In addition, the prevalence of mask-wearing decreased as the Townsend deprivation index category increased, i.e., the mask-wearing was less prevalent in lower socioeconomic areas. High-deprivation areas were also more likely to have higher percentages of partial mask-wearing than low-deprivation areas.
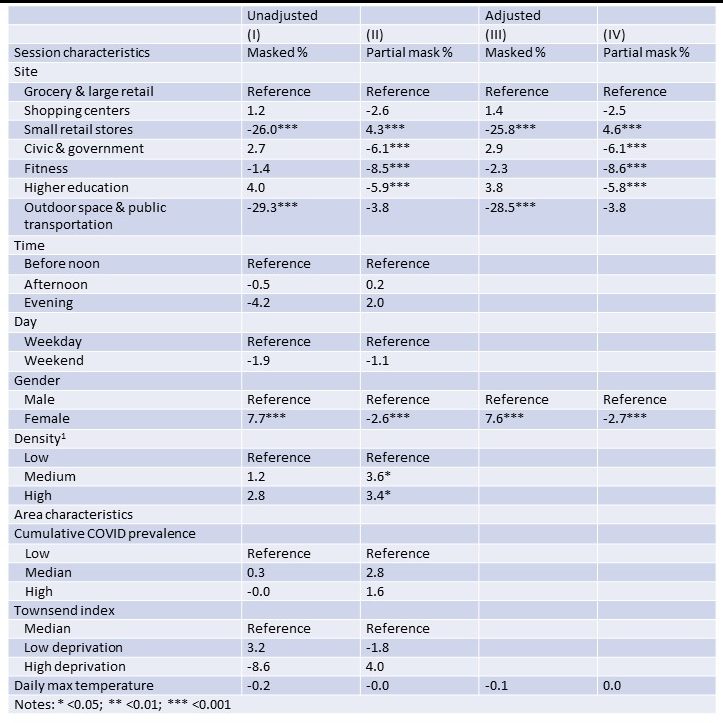
In the adjusted regression models (Table 2 and Appendix 2), the probability of mask-wearing was about 26 percentage points lower in small retail stores and 29 percentage points lower in outdoor spaces and public transportation in comparison to grocery and large retail stores (Column III). For partial mask-wearing, more variation was observed across site types (Column IV). Compared to grocery and large retail stores: partial mask-wearing was nearly 9 percentage points higher in fitness locations; nearly 5 percentage points higher in small retail stores than grocery and large retail stores; 6 percentage points lower in civic and government locations; and 5% lower in higher education locations. Females were associated with more mask-wearing than males (nearly 8 percentage points higher). Males had a nearly 3 percentage point higher prevalence of partial mask-wearing.
Mask-wearing in public is an important preventative public health measure to address the COVID-19 pandemic, particularly in the absence of effective therapeutics and widespread vaccination. We observed that a majority of people wear masks in public. Our estimate of more than 80% correct masking in indoor locations is generally consistent with self-reported data also suggesting a majority people wear masks in public (Bruine de Bruin et al., 2020; Hornik et al., 2020; Hutchins et al., 2020; Igielnik, 2020; Kramer, 2020; Sheehan et al., 2020) as well as observational studies of specific populations and settings (Arp et al., 2020; Barrios et al., 2021; Haischer et al., 2020; West Virginia University, School of Public Health, 2021). While public health professionals and agencies encourage universal mask-wearing, this level of mask-wearing is very encouraging as simulation studies estimate that rates of at least 80% may be sufficient to reduce the spread of COVID-19 (Eikenberry et al., 2020; Kai et al., 2020). Nevertheless, we observed important variations in the prevalence and correctness of mask-wearing.
Notably, this is among the first studies to distinguish between and report correct and incorrect mask-wearing by the general population in a wide variety of public settings (Arp et al., 2020; Barrios et al., 2021; Haischer et al., 2020; West Virginia University, School of Public Health, 2021). Partial mask-wearing and non mask-wearing may represent different behaviors or root causes and, as such, require different interventions to effectively address. Partial mask-wearing was more common among men and in smaller retail sites. It is possible that partial mask-wearing may be due in part to lack of education on proper wearing technique or mask selection. However, the World Health Organization, federal and state public health agencies, health care organizations, celebrities and media outlets have provided substantial educational and promotional information about correct mask-wearing (CDC, 2020; Lee, 2020; WHO, 2021). Furthermore, many of our larger observation sites included signage with graphics illustrating correct usage, as did shopping centers and government and civic sites. Alternatively, partial mask-wearing may be an example of minimally compliant behavior; either to appear socially acceptable (Betsch et al., 2020) or to appear to meet the requirements of large retail chains, many of which require patrons to wear masks (Friedman, 2020). While this study did not formally document the public health messaging around mask-wearing or mask enforcement policies at any location sites, larger retail sites tended to have more prominent mask requirement signage (e.g., banners on the buildings), staff at the entrance to remind patrons, masks provided at the door, or public service announcements made within the store. These sorts of prompts and interventions were not as prominent or common at smaller retail locations, which may explain the higher prevalence of partial- and non mask-wearing observed in smaller retail stores. If partial mask-wearing is a product of a minimal compliance to meet social norms, encouraging change may be harder than education.
Differences in behavior by gender and site characteristics were also notable. First, males were less likely to correctly wear a mask in public than females. Other studies using direct observation methods have also found that females are more likely to wear masks than males (Arp et al., 2020; Haischer et al., 2020; Studio Ludo, 2020). Our observations of public behavior cannot explain the factors motivating lower mask usage among males; however, other research reports males may perceive themselves as at less risk for infection (Bruine de Bruin et al., 2020), consider non-pharmaceutical interventions to be less effective (Kasting et al., 2020), or believe that mask-wearing is an infringement on personal freedom (Howard, 2021). The differences in observed behavior in this study and the aforementioned explanations from other research suggest that targeted public health messaging may be necessary to increase mask-wearing behavior among men. Variations in behavior based on type of site were also significant. We observed higher rates of mask-wearing indoors compared to outdoor locations. This difference in behavior is consistent with Indiana State public health orders, which at the time of this study required masks indoors at all times and outdoors only when social distancing was not possible (State of Indiana, 2020). Such policy aligns with federal recommendations (CDC, 2020). Higher rates of mask usage were observed at locations that were part of national chains or large organizations like grocery stores, “big box” retailers, shopping malls, civic and government sites, or higher education settings. The high level of mask-wearing at these locations may be partially attributable to enforcement. As previously noted, numerous large retail chains make mask-wearing a matter of corporate policy (Friedman, 2020) and likewise universities have established requirements for student, staff and faculty behavior on campus (Barrios et al., 2021). In contrast, fitness locations had higher percentages of non mask-wearing, which may be in response to individuals’ perceived discomfort wearing masks during exercise (Mallenbaum, 2020).
Ongoing observation of public mask-wearing behavior provides valuable, real-time information that can be used to target public health interventions and responses. For one, enforcement of mask mandates has generally been uneven in the United States and much of the enforcement has been left up to private businesses (Gee & Gupta, 2020). For businesses and other sites, these findings can be used to help establish face masks as normal and expected behavior. For example, businesses and other sites could tailor signs or in-store announcements to highlight that the vast majority, more than 8 out of 10, people correctly wear masks at their location. As mask-wearing in public becomes the norm, individual wearing of masks generally increases (Barceló & Sheen, 2020). Communities should do all they can to increase the overall acceptance of mask-wearing, and mask-wearing should increase. Public health agencies can make similar use of these results to reinforce behavioral norms and to customize and target their messaging, such as requiring masks in all indoor locations regardless of the size or purpose of the business. Masks continue to be a critical public health tool as many people have yet to be vaccinated, and we still do not know the extent to which vaccines will reduce transmission. As vaccination rates increase, it is possible that compliance with masking recommendations will decrease. Reliable measurements of mask use may be an invaluable tool in continued efforts to reduce transmission of SARS-CoV-2.
This study has several limitations. First, we were unable to collect robust demographic data using direct observation methods. We did not believe that observers could reliably infer characteristics such as age, race or ethnicity without bias, and our assignments of individual sex may have been incorrect in some cases. Second, because we did not directly engage with individuals, we have no measures of motivation or perceptions about COVID-19, mask-wearing or other public health practices. Mask behaviors do vary by age, with younger adults less likely to wear masks (Haischer et al., 2020). However, we included a set of sites dominated by younger adults: higher education, where the prevalence of mask-wearing was no different than other public settings. Similarly, we did not systematically characterize the educational and enforcement activities at each observation site. Finally, generalizability is limited. Marion County has been responsive with mask mandates and public health measures during the pandemic and the state of Indiana had a concurrent mask mandate throughout the study period. These were largely constant during our study period (e.g., mask mandates had been in place for months prior), but we collected data during some of the highest points of the outbreak in the United States (The New York Times, 2021). Likewise, while we observed a variety of sites, these locations may be very different from other types of locations in Marion County or elsewhere. For example, we did not include restaurants or food courts, given the limitations of assessing mask behavior while individuals eat and drink. Likewise, Marion County is an urban setting, so that we did not observe settings in rural locations.
The majority of people wore face masks correctly in public and at levels that may help arrest the spread of COVID-19 and establish mask-wearing as normal, expected behavior. Continual collection of reliable mask behavior data can support private businesses and public health agencies in encouraging compliance.
This work was made possible through funding by the Bloomberg Philanthropies. The authors thank Nicholas Kiehl, Brooke Nine, Brayton Nyland, Elizabeth Reedy, Lexie Perkins, Gracie Tial, Lauren Yoder, Wenny Zheng.

Joshua R. Vest, PhD, MPH is the Director of the Indiana University Richard M. Fairbanks School of Public Health at Indianapolis’ Center for Health Policy, a Professor and Vice-Chair of Health Policy & Management, and a Research Scientist with the Regenstrief Institute.. He is a health services researcher and former state and local public health practitioner.
Shama Cash-Goldwasser, MD, MPH, a physician and epidemiologist, is senior technical advisor on the Prevent Epidemics team at Resolve to Save Lives, an initiative of Vital Strategies.
Elhaam Bandali’s educational background encompasses an MS in Nutritional Health Sciences and a subsequent MPH in Epidemiology. Bandali currently works as a Program Management Specialist at the Indiana University Richard M. Fairbanks School of Public Health, Center for Health Policy. Her role has involved working on multiple research projects including surveillance of face mask usage during the COVID-19 pandemic in Marion County, Indiana and surveillance of opioid use after traumatic injury in adolescents in Indiana.
Dr. Peters Bergquist has over 20 years of experience working in the field of infectious disease control, including prevention, treatment, care, immunization, and epidemiology. She holds a PhD in Global Health/Public Health Studies (Behavioral Science), an MSPH in Tropical Medicine, and an MA in Medical Anthropology. She also teaches graduate and undergraduate global health and anthropology of infectious disease courses.
Dr. Paul Halverson is the founding dean of the Indiana University Richard M. Fairbanks School of Public Health. His career includes appointments as the Arkansas state health officer and director of health, senior management roles at the US Centers for Disease Control and Prevention, and senior policy advisor for the North Carolina Department of Environment, Health and Natural Resources. He is an experienced national leader having served on the boards of many national and international organizations and efforts. His research efforts focus on public health systems and services research bridging evidence and public health practice. His work focuses on protecting and improving the health of vulnerable populations through health policy, business, policy, informatics and advocacy.
Dr. Peter Embí is an internationally recognized researcher, educator, and leader in the field of biomedical and health informatics, with numerous peer-reviewed publications and presentations describing his innovations in the field. His areas of interest include clinical & translational research informatics, public health informatics, health information technology, informatics ethics, and learning health systems.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()