
Irfan A, Bieniek-Tobasco A, Golembeski C. Pandemic of racism: public health implications of political misinformation. Harvard Public Health Review. 2021; 26.
DOI:10.54111/0001/Z6
Misinformation amplified by political elites can lead to an increase in racism and discrimination against racial and ethnic minorities and other populations who experience vulnerabilities. Politically-motivated misinformation, as observed during the COVID-19 pandemic, can have far-ranging public health consequences, including negative physical and emotional health outcomes. Misinformation, political or otherwise, and racist rhetoric must be categorically rejected. Scientists and the general public have a moral duty to advocate against and repudiate the racialization of disease and racist speech in all forms (Yore, 2020).
In the midst of the current COVID-19 pandemic, inflammatory and racist rhetoric driven and encouraged by misinformation poses additional public health risks. In a crisis, fear is a natural response. Pandemics are no exception. However, fear in an environment of political misinformation can lead to mistrust, inability to determine factual information, and surges in racially driven discrimination or violence as is being witnessed today in the United States. Negative emotions can spread like a contagion (Kramer et al., 2014) and politicians condoning inflammatory rhetoric can encourage such racially motivated prejudice in a society (Newman et al., 2020). In the case of COVID-19, the spread of deliberate political misinformation has been amplified by some of our political elites, especially against Asians and Asian Americans. The likely adverse effects of this political misinformation are visible in the latest data from Stop AAPI Hate, (APPPC, 2020) a collaborative project of the Asian Pacific Policy & Planning Council that collects and reports anti-Asian American and Pacific islander hate violence, adult harassment, discrimination, shunning, and child bullying. The data suggest an increase in hate crimes against Asian Americans with more than a thousand incidents reported in just a matter of days after the project launch. Stop AAPI Hate has been issuing weekly reports (STOP AAPI HATE Reports, 2020) on incidents of coronavirus discrimination that include being barred from establishments and transportation; coughed or spat upon; verbally harassed; physically assaulted; harassed online; shunned; vandalized; and discriminated against in the workplace. Political misinformation that implies a specific group is responsible for a pandemic, and “otherist” rhetoric elevate and motivate racism and will likely have negative impacts far beyond the current crisis.
Some political leaders have been spreading misinformation with racist undertones and identifying COVID-19 and SARS-CoV-2 as a ‘foreign,’ (CNN, 2020), ‘Chinese,’ (Fallows, 2020) ‘Wuhan,’ (King et al., 2020) and ‘Kung Flu’ (Rogers et al., 2020) virus, while neglecting to prioritize an expeditious response and focus toward expanding public health protections and healthcare access during the crisis (Ho, 2020). Claims that this is a typical and accepted way to name novel diseases are incorrect (WHO, 2015), and this language has real life-threatening consequences for real people (Tavernise & Oppel Jr., 2020). Even though certain diseases have been named after geographic areas in the past, the World Health Organization now explicitly prohibits it to “avoid causing offence to any cultural, social, national, regional, professional or ethnic groups” (WHO, 2015). Whatever the reasons behind this use of language are, we argue that labeling a disease in a way that targets a group of people is a form of misinformation, however unintentional, that not only detracts from crucial public health responses and messaging but causes further harm to population health while exacerbating health inequities.
Racism and discrimination are institutionalized in the U.S. Structural racism, which reinforces discriminatory beliefs, values, and resource distribution, has been defined as “the totality of ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care, and criminal justice” (Bailey et al., 2017). Discrimination, including microaggressions and violence, may discourage vulnerable populations from seeking care, participating in contact tracing, or adopting public health-protective behaviors. Furthermore, racism has been tied to negative physical and mental health impacts. Institutional and interpersonal discrimination are determinants of health outcomes and health disparities (Davis, 2020). Adverse health outcomes associated with various forms of racism include hypertension, diabetes, obesity, stress, and low-birth-weight (Williams et al., 2019). According to the U.S. Department of Health and Human Services, in general, mortality rates for heart disease, stroke, cancer, asthma, influenza, pneumonia, diabetes, and HIV/AIDS are disproportionately higher for Black Americans in comparison to whites (HHS, n.d.), for instance.
Social-structural drivers of health inequities, amidst the COVID-19 pandemic, include reliance on public transit, working on the frontline, less autonomy, reliance on more crowded living and workspaces, and the inability to work from home. Dr. Lisa Bowleg cautions against obscuring “structural inequities that befall Black and other marginalized groups, who bear the harshest and most disproportionate brunt of anything negative or calamitous: HIV/AIDS, hypertension, poverty, diabetes, climate change disasters, unemployment, mass incarceration, and, now, COVID-19” (Bowleg, 2020). Disproportionate levels of severe COVID-19 (Garg et al., 2020) and death (Ray, 2020) among Black Americans is a stark representation of centuries of structural and cultural racism, including unequal healthcare access and quality (Feagin & Bennefield, 2014). Some of the underlying conditions that increase the risk of severe manifestations and complications of COVID-19 are the same adverse health outcomes associated with experiencing racism. Additionally, fear and experienced racism may also impact the ability of Black Americans to safely participate in protective or preventative behaviors such as wearing masks (Weingartner, 2020).
We also acknowledge the methodological challenges in measuring racism and the inadequacies of reducing race or ethnicity to a single categorical variable. It is very likely that current research quantifying these health impacts underestimates the health impacts of racism and the impact of self-reported experiences of discrimination on mental and physical health (Lewis et al., 2015). In the context of COVID-19, Ruha Benjamin best describes the interconnectedness of biological diseases and inequitable societal structures by highlighting that “the virus is not simply a biological entity, but a biopolitical reality which travels along well-worn patterns of inequity” (Benjamin, 2020).
Discriminatory attitudes and practices toward Asians and Asian Americans within a public health context is not a new phenomenon. In her book, Fit to be Citizens?, Natalia Molina describes: “By the 1870s, public health officials had sufficient credibility to construct what being ‘Chinese’ meant—namely, dirty, depraved, and disease-ridden. These stereotypes, in turn, justified segregating Chinese people so that they would not taint white city residents” (Molina, 2006). These grotesque stereotypes and racist views continue to be reflected contemporarily through covert misinformation. The racist overtones of past quarantine practices are reflected in Dr. Mary Sawtelle’s 1878 remarks in a medical journal suggesting Chinese immigrants purposefully spread “germs of death to another better race” (Shah, 2003). Centuries later, these dehumanizing views continue to survive and thrive as a result of racist misinformation campaigns, even if these are designed to deflect blame from leadership failure. In San Francisco, Chinese residents were disparagingly characterized as vectors of infectious disease or illness, literally quarantining them with barbed wires (Lamar, 2012), partly fueling the 1882 Chinese Exclusion Act and prompting cruel, debilitating quarantining practices based on Sinophobic sentiments rather than empirical evidence. In contrast, the white residents in the same area had no movement restrictions. These are just a few examples and a reminder of how racist rhetoric and political misinformation take hold and lead to a collective social consciousness justifying the unthinkable human rights abuses through public policies.
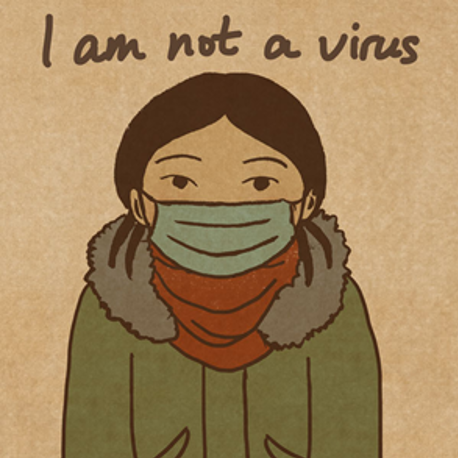
Western bigotry towards Asian Americans is not a nascent phenomenon. The specter of the ‘yellow peril’ (Tchen & Yeats, 2014) loomed large then and continues today as French newspapers declared: “Alerte jaune” (translation: Yellow alert) and “Le péril jaune?” (translation: The yellow peril?) in response to COVID-19 (Thiessen, 2020). These mainstream headlines are reflective of a societal tolerance of bigotry and discrimination towards racial and ethnic minorities. In 2003, Iris Chang suggested that UC Berkeley’s ban on students from some Asian countries reflects the ease by which excessive fears of SARS can contribute to discrimination against Asians (Chang, 2003). Just this February 2020 UC Berkeley University Health Services Center apologized and removed a social media post regarding potential “common reactions” to COVID-19 after receiving criticisms that the post normalized racism in suggesting “prejudice against people from other countries” might constitute such a “common reaction” (Deese, 2020). This covert, inadvertent, and overt racism has inspired activism among Asian American communities, including through arts (Figure 1).
This thread of misinformation-driven racism continues in the media’s discussion of ‘wet markets’ with calls to ban ‘wet markets’(Wise, 2020) due to the risk of zoonotic diseases instead of calling for evidence-based regulations. Wet markets are a critical part of the food systems in many countries. This paranoia may undermine the cultural and food security importance of these markets, which play a similar role as farmers’ markets in the U.S., providing fresh produce and meat. To make a comparison in the American context, imagine the absurdity of a Congressional legislative proposal banning farmers’ markets in the U.S., particularly in areas where it is not common to find fresh food or full grocery stores. Moreover, diseases related to food systems such as zoonotic and food-borne illnesses are not unique to the wet markets. In the U.S., deer hunting and factory farms are associated with the spread of diseases such as tuberculosis (Sunstrum et al., 2019) and antibiotic-resistant bacteria (Silbergeld et al., 2008), respectively. Lynteris and Fearnley trace this 21st-century emergence of moral panic and warn against permanently closing ‘wet markets’ due to potential adverse public health outcomes, such as bolstering unregulated black markets and destroying a food sector accounting for 30-59% of Chinese consumers’ food supplies (Lynteris & Fearnley, 2020; Maruyama et al., 2016). While there are valid and important public health concerns around the operation of some of these markets, these are no different than the risks associated with factory farms, etc., and the evidence-based regulations and diplomacy are more effective tools than the otherist and racist language, attitudes, and policy proposals.
We invite policymakers, government officials, scientists, and the healthcare workforce to take advantage of this moment to reflect on potential misconceptions, acquire cultural humility and structural competencies as part of undoing the perpetuation of intellectual and cultural colonialism. The public health and broader scientific communities should condemn racism against Asians and Asian Americans without reservation. In our day-to-day conversations, we should call out our loved ones, friends, and leaders any time they engage in “casual racism,” ‘jokingly’ from dinner tables, tweets, memes, group messages, or podiums. Moreover, the critical need for engaging community members to be involved in responding to the pandemic and any public health messaging, as Dr. Uché Blackstock underscores, has never been more urgent (King, 2020). Inclusive approach to this pandemic is the key to success, as former New York City Health Commissioner Dr. Mary Bassett said “We are only as safe as our most vulnerable citizen” (FXB Center, 2020).
Words matter. Racist rhetoric rooted in political misinformation that vilifies entire cultures is a political leadership failure and an affront to this nation’s public health response. Concerted efforts toward dismantling structural racism, and its impact on population health, must be a core part of the response and addressing the impacts of this pandemic. Racist and discriminatory rhetoric, which racializes certain diseases and health conditions, is in direct opposition to that priority and puts lives at risk. We must speak up and hold our political and public health leadership accountable for a dignified public discourse and equitable public health policies.
“In the end, we will remember not the words of our enemies, but the silence of our friends.”
Dr. Martin Luther King, Jr. (“Trumpet of Conscience”, n.d.) Tweet
APPPC. (2020). STOP AAPI HATE. A3PCON – ASIAN PACIFIC POLICY and PLANNING COUNCIL. Retrieved 14 August 2020, from https://www.asianpacificpolicyandplanningcouncil.org/stop-aapi-hate/.
Bailey, Z., Krieger, N., Agénor, M., Graves, J., Linos, N., &
Bassett, M. (2017). Structural racism and health inequities in the USA: evidence and interventions. The Lancet, 389(10077), 1453-1463. https://doi.org/10.1016/s0140-6736(17)30569-x.
Benjamin, R. (2020). Black Skin, White Masks: Racism, Vulnerability & Refuting Black Pathology. Department of African American Studies. Retrieved 20 April 2020, from https://aas.princeton.edu/news/black-skin-white-masks-racism-vulnerability-refuting-black-pathology.
Bowleg, L. (2020). We’re Not All in This Together: On COVID-19, Intersectionality, and Structural Inequality. American Journal Of Public Health, 110(7), 917-917. https://doi.org/10.2105/ajph.2020.305766.
Chang, I. (2003). Fear of SARS, Fear of Strangers. Nytimes.com. Retrieved 14 August 2020, from https://www.nytimes.com/2003/05/21/opinion/fear-of-sars-fear-of-strangers.html.
CNN. (2020). READ: Trump’s Oval Office speech on the coronavirus outbreak. CNN. Retrieved 14 August 2020, from https://www.cnn.com/2020/03/11/politics/read-trump-coronavirus-address/index.html.
Davis, B. (2020). Discrimination: A Social Determinant Of Health Inequities. https://doi.org/10.1377/hblog20200220.518458,
Deese, K. (2020). UC Berkeley, others accused of fueling racism amid Coronavirus outbreak. TheHill. Retrieved 14 August 2020, from https://thehill.com/homenews/news/481025-uc-berkeley-gets-backlash-for-coronavirus-reaction-post.
Fallows, J. (2020). The ‘Chinese Virus’: 2020 Time Capsule #5. The Atlantic. Retrieved 14 August 2020, from https://www.theatlantic.com/notes/2020/03/2020-time-capsule-5-the-chinese-virus/608260/.
Feagin, J., & Bennefield, Z. (2014). Systemic racism and U.S. health care. Social Science & Medicine, 103, 7-14. https://doi.org/10.1016/j.socscimed.2013.09.006.
FXB Center. (2020). Dr. Mary T. Bassett’s Statement on COVID-19 for the Poor People’s Campaign. FXB Center for Health & Human Rights | Harvard University. Retrieved 14 August 2020, from https://fxb.harvard.edu/2020/04/01/dr-mary-t-bassetts-statement-on-covid-19-for-the-poor-peoples-campaign/.
García, S. (2020). ‘I am not a virus.’ How this artist is illustrating coronavirus-fueled racism. PBS NewsHour. Retrieved 14 August 2020, from https://www.pbs.org/newshour/arts/i-am-not-a-virus-how-this-artist-is-illustrating-coronavirus-fueled-racism.
Garg, S., Kim, L., Whitaker, M., O’Halloran, A., Cummings, C., & Holstein, R. et al. (2020). Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020. Retrieved 14 August 2020, from.
HHS.
Black/African American – The Office of Minority Health. Minorityhealth.hhs.gov. Retrieved 14 August 2020, from https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=61.
Ho, C. (2020). Medicaid for All Who Face the Coronavirus. Retrieved 14 August 2020.
King, D., Baptiste, N., Rosenberg, J., & Rosenberg, J. (2020). We shouldn’t need to explain why Trump’s “Chinese virus” tweet is wrong. But here we are.. Mother Jones. Retrieved 14 August 2020, from https://www.motherjones.com/media/2020/03/republican-racist-label-coronavirus/.
King, J. (2020). Uché Blackstock: We Must Do Better on COVID-19 Messaging in Black Communities. Mother Jones. Retrieved 14 August 2020, from https://www.motherjones.com/politics/2020/08/er-doctor-we-must-do-better-on-covid-19-messaging-in-black-communities/.
Kramer, A., Guillory, J., & Hancock, J. (2014). Experimental evidence of massive-scale emotional contagion through social networks. Proceedings Of The National Academy Of Sciences, 111(24), 8788-8790. https://doi.org/10.1073/pnas.1320040111.
Lamar, C. (2012). In 1900, San Francisco’s Chinatown was quarantined with barbed wire fences. io9. Retrieved 14 August 2020, from https://io9.gizmodo.com/in-1900-san-franciscos-chinatown-was-quarantined-with-5878877.
Lewis, T., Cogburn, C., & Williams, D. (2015). Self-Reported Experiences of Discrimination and Health: Scientific Advances, Ongoing Controversies, and Emerging Issues. Annual Review Of Clinical Psychology, 11(1), 407-440. https://doi.org/10.1146/annurev-clinpsy-032814-112728.
Lynteris, C., & Fearnley, L. (2020). Why shutting down Chinese ‘wet markets’ could be a terrible mistake. The Conversation. Retrieved 14 August 2020, from https://theconversation.com/why-shutting-down-chinese-wet-markets-could-be-a-terrible-mistake-130625.
Maruyama, M., Wu, L., & Huang, L. (2016). The modernization of fresh food retailing in China: The role of consumers. Journal Of Retailing And Consumer Services, 30, 33-39. https://doi.org/10.1016/j.jretconser.2015.12.006.
Molina, N. (2006). Fit to Be Citizens?. University of California Press. Retrieved 14 August 2020, from https://www.ucpress.edu/book/9780520246492/fit-to-be-citizens.
Newman, B., Merolla, J., Shah, S., Lemi, D., Collingwood, L., & Ramakrishnan, S. (2020). The Trump Effect: An Experimental Investigation of the Emboldening Effect of Racially Inflammatory Elite Communication. British Journal Of Political Science, 1-22. https://doi.org/10.1017/s0007123419000590.
Ray, R. (2020). Why are Blacks dying at higher rates from COVID-19?. Brookings. Retrieved 14 August 2020, from https://www.brookings.edu/blog/fixgov/2020/04/09/why-are-blacks-dying-at-higher-rates-from-covid-19/.
Rogers, K., Jakes, L., & Swanson, A. (2020). Trump Defends Using ‘Chinese Virus’ Label, Ignoring Growing Criticism. Nytimes.com. Retrieved 14 August 2020, from https://www.nytimes.com/2020/03/18/us/politics/china-virus.html.
Shah, H. (2003). “Asian Culture” and Asian American Identities in the Television and Film Industries of the United States. Semanticscholar.org. Retrieved 14 August 2020, from https://www.semanticscholar.org/paper/%E2%80%9CAsian-Culture%E2%80%9D-and-Asian-American-Identities-in-of-Shah/1f3eb9f7848810dd091d447d5d22d867e6a4445c.
Silbergeld, E., Graham, J., & Price, L. (2008). Industrial Food Animal Production, Antimicrobial Resistance, and Human Health. Annual Review Of Public Health, 29(1), 151-169. https://doi.org/10.1146/annurev.publhealth.29.020907.090904.
STOP AAPI HATE Reports. (2020). STOP AAPI HATE Reports. A3PCON – ASIAN PACIFIC POLICY and PLANNING COUNCIL. Retrieved 14 August 2020, from http://www.asianpacificpolicyandplanningcouncil.org/stop-aapi-hate-reports/.
Sunstrum, J., Shoyinka, A., Power, L., Maxwell, D., Stobierski, M., & Signs, K. et al. (2019). Notes from the Field: Zoonotic Mycobacterium bovis Disease in Deer Hunters — Michigan, 2002–2017. Retrieved 14 August 2020, from.
Tavernise, S., & Oppel Jr., R. (2020). Spit On, Yelled At, Attacked: Chinese-Americans Fear for Their Safety. Nytimes.com. Retrieved 14 August 2020, from https://www.nytimes.com/2020/03/23/us/chinese-coronavirus-racist-attacks.html.
Tchen, J., & Yeats, D. (2014). Yellow Peril: 19th-Century Scapegoating. Asian American Writers’ Workshop. Retrieved 14 August 2020, from https://aaww.org/yellow-peril-scapegoating/.
Thiessen, T. (2020). France In Grips Of Racism Epidemic, As Coronavirus Fans Anti-Asian Hysteria. Forbes. Retrieved 14 August 2020, from https://www.forbes.com/sites/tamarathiessen/2020/02/11/france-in-grips-of-racism-epidemic-as-coronavirus-fans-anti-asian-hysteria/#4c23980452d7.
Trumpet of Conscience. The Martin Luther King, Jr., Research and Education Institute. Retrieved 14 August 2020, from https://kinginstitute.stanford.edu/encyclopedia/trumpet-conscience.
Weingartner, T. (2020). For Black Americans, Following CDC Mask Guidelines Can Be A Fraught Decision. Wvxu.org. Retrieved 14 August 2020, from https://www.wvxu.org/post/black-americans-following-cdc-mask-guidelines-can-be-fraught-decision#stream/0.
WHO. (2015). WHO | WHO best practices for naming of new human infectious diseases. Who.int. Retrieved 14 August 2020, from https://www.who.int/topics/infectious_diseases/naming-new-diseases/en/.
Williams, D., Lawrence, J., & Davis, B. (2019). Racism and Health: Evidence and Needed Research. Annual Review of Public Health, 40(1), 105-125. https://doi.org/10.1146/annurev-publhealth-040218-043750.
Wise, J. (2020). Bipartisan lawmakers call for global ‘wet markets’ ban amid coronavirus crisis. TheHill. Retrieved 14 August 2020, from https://thehill.com/homenews/senate/491948-bipartisan-lawmakers-call-for-global-ban-of-wet-markets-due-to-coronavirus.
Yore, H. (2020). Coronavirus and HIV Parallels: On Racializing and Queering Illness. Advocate.com. Retrieved 14 August 2020, from https://www.advocate.com/commentary/2020/2/26/coronavirus-and-hiv-parallels-racializing-and-queering-illness.
Ans Irfan is a multidisciplinary global public health expert with over a decade of experience in advancing global health equity. He currently serves as a faculty member and Director for the Climate & Health Equity Practice Fellowship at George Washington University. He is also a fellow with the Robert Wood Johnson Foundation Health Policy Research Scholars program. As a critical public health scholar, entrepreneur, and scientist he combines multiple disciplines through a multimethod approach to provide innovative interdisciplinary public policy and programmatic solutions geared towards ameliorating social and health inequities.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()