Miller L, Joachim-Célestin M, Lara M, Deshields S, DaCosta Davis S, Montgomery S, Clarke C. Acculturation, familial support, and unhealthful dietary patterns: evaluating notable trends in a Latino population. Harvard Public Health Review. 2019;23.
DOI:10.54111/0001/W1
Increased acculturation among Latinos has been associated with a decrease in the quality of dietary habits and an increase in the prevalence of obesity. The aim of this pilot study was to compare the consumption of fast/processed foods and sugary beverages in Spanish speaking vs. non-Spanish speaking Hispanics and those born in the United States with immigrants. We also explored the degree of familial support individuals received for incorporating healthy lifestyle habits across acculturation levels. Surveys were completed by 50 Hispanic community participants residing in Southern California. Questions pertaining to acculturation, eating habits, and familial support were analyzed for frequency and correlational significance via SPSS v. 24. Analyses revealed a statistically significant difference in the frequency of consumption of fast food/packaged food across both units of analysis: being born in the United States and speaking predominantly English correlated with greater consumption of fast and processed food (both p<.001). Although the difference was only marginally significant, sugary drink consumption tended to also be associated with US birth (p=.06). The protective effect of speaking Spanish at home and being born outside of the US was moderate (r=.42 and r=.59, respectively). On the other hand, the amount of perceived familial support for physical activity/healthy dietary patterns was not associated with language spoken at home nor country of birth. This study confirms previous research that demonstrates that acculturation promotes obesogenic dietary habits among Latinos.
Latinos are the fastest growing minority group in the United States and currently make up nearly 17.8% of the population (US Census Bureau, 2010). Studies show rising rates of overweight and obesity among both Latino children and adults (38.9% of children, 77.1% of adults). They also have higher rates than their non-Hispanic white (28.5% of children, 68.5% of adults) and non-Hispanic black (35.2% of children,76.3% of adults) counterparts (Ogden, Carrol, Kit & Flegal, 2014). Obesity poses a threat to the overall health and well-being of the Latino community. It is also associated with an increased risk of cardiovascular disease, metabolic syndrome, type 2 diabetes, hypertension, and certain forms of cancer (Pi-Sunyer, 2002).
Current research suggests that acculturation, defined as the extent to which one adopts values, behaviors, lifestyle, and language of the local culture, may play an important role in the increasing rates of obesity observed. Studies also show that increased acculturation is associated with increased intake of high fat foods and a decreased frequency of physical activity (Montez & Eshbach, 2008).
The purpose of this study was to evaluate certain lifestyle behaviors related to dietary and physical exercise habits of Latinos residing in two southern California counties, and to identify correlations between these behaviors and acculturation.
Procedures: The cross-sectional pilot study was conducted at a small food distribution center set in a community church in preparation for a community health worker (promotores) facilitated weight loss program. Specifically, the survey explored cultural barriers to weight loss participation in bi- and mono-lingual overweight Latinos to inform a more culturally aligned curricula development. The food distribution center was established in addition to free weekly half day on-site health care sessions in response to patient’s indication of high levels of food insecurity. Bilingual and monolingual Latino participants were recruited from the food distribution center to take part in the pilot survey. Participants received a $20 gift card in exchange for their completion of the survey. Study procedures were approved by the Loma Linda University Institutional Review Board.
Measures: The study used a survey to evaluate the demographics and lifestyle habits of Latinos residing in the counties of Riverside and San Bernardino, CA. Terminology for questions on food frequency were modeled after the NHANES Food Questionnaire adapting for participants personal and cultural definitions. These definitions were obtained through focus group data in which participants were asked how they would classify “sugary drinks” and “fast or packaged foods.” Using their wording and examples for justification, consumption of fast/packaged foods was determined based on the response to the question “Over the last 2 weeks, how often have you eaten the following: fast food or packaged foods (e.g., chips, candy, cracker, cookies)?” For sugary drinks, the question was “Over the last 2 weeks, how often have you drunk the following: sugary drinks (e.g., soda, sports drinks, juice)? A 4-point Likert scale was used to measure both questions, answers included: “never or rarely,” “sometimes,” at least half of the days,” and “almost every day.”
Social support was assessed by asking participants four questions: “Over the past 3 months, how often did your family members do the following to/with you?”: “eat healthy food such as fruits, vegetables, food and low fat, low salt and low sugar foods?” “Encourage you to quit eating unhealthy or junk food?” “Encourage you to engage in physical activity?” “Engage in physical activity or went for a walk with you?” Possible answers included: “never or rarely,” “sometimes,” “many times,” “almost always.”
Analytic Methods: Descriptive analyses included frequency counts for country of birth, language, dietary habits, and social support for dietary habits. For the 4-point Likert scales described above, frequency was measured based on the allocation of a numeric value to the answers where “never or rarely” = 1, and “almost every day/always” = 4. Because some of the options for social support had few answers, answers were merged to produce a dichotomous variable. Finally, answers to the question assessing birth country were also merged into two categories (US born and born in another country) since most participants born outside of the US were born in Mexico. Differences in behavior and social support, and association between variables were analyzed via SPSS v.24 using Mann-Whitney and Kruskal-Wallis tests, and Spearman Rank Correlation.
Participant demographics are summarized in Table 1. Participants were 18 years or older, self-identified as Latino/Hispanic and had varying degrees of acculturation. The mean age of participants was 45.5 (±16.91) years of age. A majority (70%) of the participants were female (n=35), and most participants were born in Mexico or a South American country (n=35, 70%). Furthermore, the majority (66-72%) reported reading Spanish and speaking it at home and with friends.
Graph 1 below shows US-born and immigrant participants’ responses to the “fast/packaged food” question. Overall, participants who were born in the United States reported eating fast/packaged foods more frequently than their non-US native counterparts, U=94.00, z=-4.12, p<0.001, r=-0.58.
Table 2 shows the difference in self-reported fast/packaged food and beverage consumption between participants born in the United States and those who immigrated to this country. There was an inverse correlation between birth outside of the US and frequency of fast food/packaged foods consumption (rs=-0.59, p<0.001). There was also a marginally statistically significant difference in sugary drinks consumption between these two groups (p=0.06), with those born in the US being more likely to consume sugary drinks.
Similar results were found when comparing lifestyle behavior and language (as a proxy for acculturation). Fast / packaged foods consumption was significantly affected by language spoken at home, H(2)=9.53, p<.005. Mann-Whitney tests were used as post hoc tests to determine which groups differed from one another. A Bonferroni correction was applied, so all effects are reported at a .0167 level of significance. It appears that fast/packaged food consumption was not different between those who spoke English only and those who spoke both languages at home (U=11.50, ns, r=-.18), nor between those who spoke Spanish and those who spoke both languages at home (U=63, ns, r=-.07). However, fast/packaged foods consumption was significantly lower among Spanish-only speakers compared to those who only spoke English at home (U=79.50, z=-3.11, p=.002, r=-.44). Therefore, the more acculturated group was more likely to consume processed/packaged foods.
Graph 2 illustrates the dose effect of speaking Spanish at home on fast food/packaged food consumption: the negative correlation between consumption of fast food/packaged food and use of the Spanish at home was moderate (rs=-0.42, p=0.003). In other words, those who spoke more English were more likely to eat fast/packaged foods than those who spoke an equal amount of English and Spanish, while the latter group consumed more fast or packaged food than those who spoke mainly Spanish at home.
There was no statistically significant difference in perceived familial support for physical activity or dietary habits between those who spoke mainly Spanish and those who spoke mainly English. In addition, there was no statistically significant difference in the amount of familial support for physical activity/dietary habits based on birth country.
Overall our results show a positive correlation between the degree of acculturation (measured by language spoken in the home and country of birth) and the frequency of fast and packaged foods consumption. Several qualitative studies report similar results and suggest reasons for these observations. Research by Ramirez, Golash-Boza, Unger and Baezconde-Garbanati (2018) involving the analysis of focus groups among Mexican American women proposed that Mexican Americans perceive the American diet to be healthier than their own. According to this same study, Mexican-Americans believe traditional Hispanic meals – i.e. rice, tacos, beans, enchiladas, pozole, ceviche, and tamales – are higher in fat and are eaten in larger portions. Despite the research showing that the US diet is characterized by large portions and high density of calories (Ramirez et al., 2018). In a 2005 study conducted on the decrease in dietary quality among acculturated Latinos, it was noted that as Latino women become more acculturated, they cook traditional Hispanic meals less frequently and opt for more fast foods for the sake of convenience (Ayala, Mueller, Lopez-Madurga, Campbell & Elder, 2005).
In addition to acculturation, several studies suggest other reasons for the increased prevalence of obesity among Latinos. While we did not directly study the effect of income and occupation on the role of dietary habits and weight management in the Latino community, a study of overweight Mexican males found that major barriers to proper weight management could be traced to the fact that many work multiple jobs, making it nearly impossible to find the time to plan, prepare, and consume healthy meals (Valdez, Amezquita, Hooker & Garcia, 2017). A similar study, of Latino parents, found that they consider healthy foods expensive and that they lack the funds to provide gym memberships and home workout programs (Taverno-Ross et al., 2018). According to Larson, Story and Nelson (2009), a possible explanation for the deterioration in dietary habits among Latinos is that residents of low income, minority, and rural neighborhoods have less access to supermarkets and of other sources of healthful food. In addition, they also tend to have the highest availability of fast food restaurants and energy-dense foods (Larson et al., 2009).
Limitations of this study included a small sample size, as this was a pilot study. Participants were also recruited from a population with food insecurity; therefore, results may not be generalizable to the entire Latino community. In addition, differences in response of the participants may have varied based on country of origin and other languages spoken in the home. Furthermore, participants were given the option of completing the survey in English or in Spanish, which introduced the possibility of slight variations in meanings/translations which could have yielded different responses among the participant groups. Another limitation is that income was not accounted for in this study. This was however decided as qualitative data because analysis of focus group qualitative data suggested that participants would not participate in the survey if such questions were addressed.
The findings of this study have important implications for addressing health challenges in a growing and vulnerable US population. Given perceptions that processed/fast American foods are healthier than traditional Mexican fare, it may be desirable for interventions to include healthy modifications to traditional meals. The misconception that healthy food is “more expensive” and “takes too long to prepare” must also be corrected.
The goal of our pilot study was to identify cultural barriers Latinos face in participating in dietary interventions and to use this information to develop a culturally adapted weight loss/lifestyle program, the “Full Plate Living,” program, in which participants are encouraged to increase their fiber consumption, while maintaining consumption of traditional foods. With knowledge from this survey indicating a high consumption of fast/packaged food among acculturated Latinos, lesson plans will focus on addressing alternatives to fast food/packaged food consumption – i.e. teaching participants how to reincorporate healthy versions of traditional Hispanic dishes into their daily routine. program is to provide a model of an obesity intervention that
Further studies should seek to evaluate the efficacy of a culturally-adapted weight loss/lifestyle program that considers the diversity of culture and cultural cuisine as a foundation for program development and implementation, focusing on decreasing the consumption of processed foods among acculturated Latino Americans.
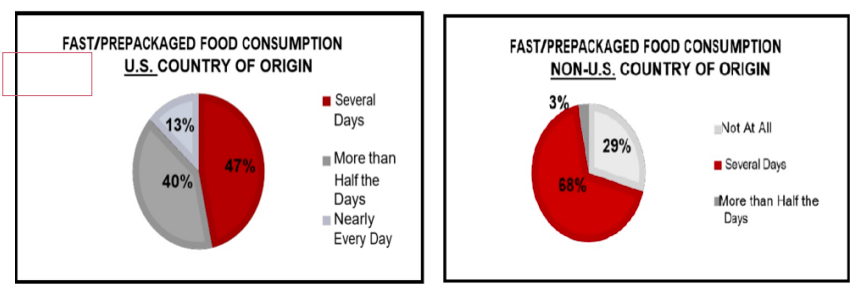
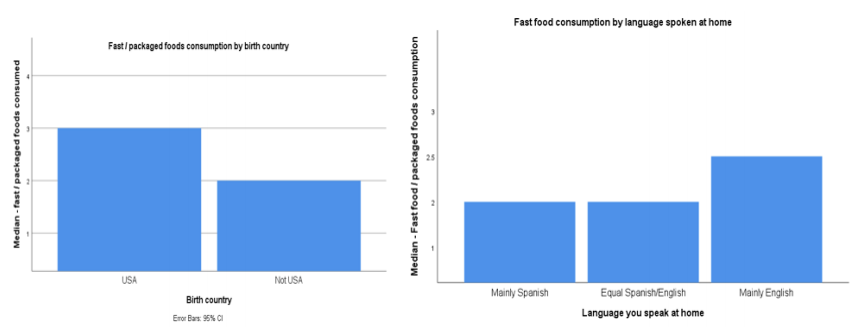
Table 1.Baseline demographics of study participants
Mean (± SD) | N (%) | |
Age (years) | 45.46 (±16.91) | |
Gender | ||
Male | 15 (30%) | |
Female | 35 (70%) | |
Country of origin | ||
Mexico/ South America | 35 (70%) | |
USA | 15 (30%) | |
Language read or spoken | ||
Mainly Spanish | 36 (72%) | |
Equal English/ Spanish | 5 (10%) | |
Mainly English | 13 (26%) | |
Language spoken at home | ||
Mainly Spanish | 36 (72%) | |
Equal English/ Spanish | 4 (8%) | |
Mainly English | 10 (20%) | |
Language spoken with friends | ||
Mainly Spanish | 33 (66%) | |
Equal English/ Spanish | 5 (10%) | |
Mainly English | 12 (24%) |
Table 2: Participants’ birth country and language spoken at home and correlations with behavior and familial social support
| Language spoken at home |
| Effect size of language N=50 | Birth Country | Effect size of birth country N=50 | ||||||
Mainly Spanish N=36 | Equal Spanish/English N=4 | Mainly English N=10 | USA N=15 | Not USA N=35 | |||||||
Mdn (±SD) | Mdn (±SD) | Mdn (±SD) | p | r | p | Mdn (±SD) | Mdn (±SD) | r | p | ||
Consumption Of… | Fast/packaged foods** | 1.82 (±0.56) | 2.00 (±0.82) | 2.63 (±0.82) | .006 | 0.42** | .003 | 2.62 (±0.72) | 2.62 (±0.72) | -0.59*** | .000 |
Sugary drinks | 1.75 (±0.90) | 2.50 (±1.29) | 2.17 (±1.06) | .31 | 0.21 | .15 | 2.33 (±1.06) | 1.71 (±0.89) | -0.26 | .06 | |
Familial social support over past 3 months | Discouraged unhealthy food | 1.67 (±0.48) | 1.75 (±0.50) | 1.80 (±0.42) | .70 | 0.12 | .40 | 1.74 (±0.46) | 1.69 (±0.47) | -0.05 | .74 |
Ate healthy food with participant | 1.89 (±0.32) | 1.75 (±0.50) | 1.90 (±0.32) | .71 | -0.03 | .85 | 1.93 (±0.26) | 1.86 (±0.36) | -0.22 | .13 | |
Encouraged PA | 1.83 (±0.38) | 1.75 (±0.50) | 1.70 (±0.48) | .63 | -0.13 | .34 | 1.67 (±0.49) | 1.86 (±0.36) | -0.11 | .45 | |
Engaged PA with participant | 1.75 (±0.44) | 1.75 (±0.50) | 1.60 (±0.52) | .65 | -0.12 | .41 | 1.67 (±0.49) | 1.74 (±0.44) | 0.08 | .59 | |
Mdn = median
r= correlation coefficient
PA = physical activity
** p value is less than 0.01 (statistically significant difference between languages or effect size of language)
*** p value is less than 0.001 (statistically significant effect of birth country on consumption of fast/packaged foods)
Ayala, G.X., Mueller, K., Lopez-Madurga, E., Campbell, N.R., & Elder, J,P. (2005). Restaurant and food shopping selections among Latino women in Southern California. Journal of the American Dietetic Association, 105 (1), 138-45.
Larson, N.I., Story, M.T., & Nelson, M.C. (2014). Neighborhood environments: disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine, 36 (1), 74-81.
Ogden, C.L., Carrol, M.D., Kit, B.K., & Flegal, K.M. (2014). Prevalence of childhood and adult obesity in the United States, 2011-2012. Journal of the American Medical Association, 311 (8), 806-14.
Montez, J.K. & Eschbach, K. (2008). Country of birth and language are uniquely associated with intakes of fat, fiber, and fruits and vegetables among Mexican-American women in the United States. Journal of the American Dietetic Association, 108(3), 473-80.
Pi-Sunyer, F.X. (2002). The obesity epidemic: pathophysiology and consequences of obesity. Obesity Research, 10 (2), 97S-104S.
Ramírez, A.S., Golash-Boza, T., Unger, J.B. & Baezconde-Garbanati,L. (2018). Questioning the Dietary Acculturation Paradox: A Mixed-Methods Study of the Relationship between Food and Ethnic Identity in a Group of Mexican-American Women. Journal of the Academy of Nutrition and Dietetics,118(3), 431-439.
Taverno Ross, S.E., Macia, L., Documet, P.L., Escribano, C., Naderi T.K. & Smith-Tapia, I. (2018). Latino Parents’ Perceptions of Physical Activity and Healthy Eating: At the Intersection of Culture, Family, and Health. Journal of Nutrition Education and Behavior, 50 (10), 968-976.
US Census Bureau. (2010). Hispanic or Latino by Type: 2010, 2010 Census Summary File 1 [Data file]. Retrieved from https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF
Valdez, L.A., Amezquita, A., Hooker, S.P., & Garcia, D.O. (2017). Mexican-origin male perspectives of diet-related behaviors associated with weight management. International Journal of Obesity (London), 41(12), 1824-1830.
Lauren E. Miller is a medical student at School of Medicine, Loma Linda University
Maud Joachim-Célestin is an adjunct instructor at School of Medicine, Loma Linda University
Marisol Lara is a research assistant at School of Public of Health, Loma Linda University
Simone Deshields is a medical student at School of Medicine, Loma Linda University
Shevel S. DaCosta Davis is a medical student at School of Medicine, Loma Linda University
Simone Deshields is a Professor and Associate Dean of Research at School of Behavioural Health, Loma Linda University
Simone Deshields is the Principal Investigator and Assistant Professor at School of Department of Medicine and Behavioural Health, Loma Linda University
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()