The Interdisciplinarian

By Sofia Weiss Goitiandia
As seen through Dalia’s eyes:
Reflections on the world of Global Health from a pioneering Sudanese activist – Part 2
For this set of articles, I interviewed Dalia Elhag, a medical doctor from Sudan, and graduate of the master’s programme in Global Health at Karolinska Institutet in Stockholm, Sweden – where I was also a student this academic year. Dalia also has a long history as an activist in the field of sexual and reproductive health and rights (SRHR), particularly in advocating against female genital mutilation (FGM), gender-based violence, and child marriage – which are all prevalent in Sudan. Dalia considers herself strongly a feminist, and feels that this is a solid basis – and inspiration – for much of her work.
The articles that follow are a written transcript of our conversations, focusing particularly on her thoughts on the kinds of contributions that can be made towards improving health equity outside of the clinic; reflections on lessons learned and challenges experienced from her (continuing) time as a young activist; as well as her perspective on what ‘decolonising’ global health means in practice.
Part 2
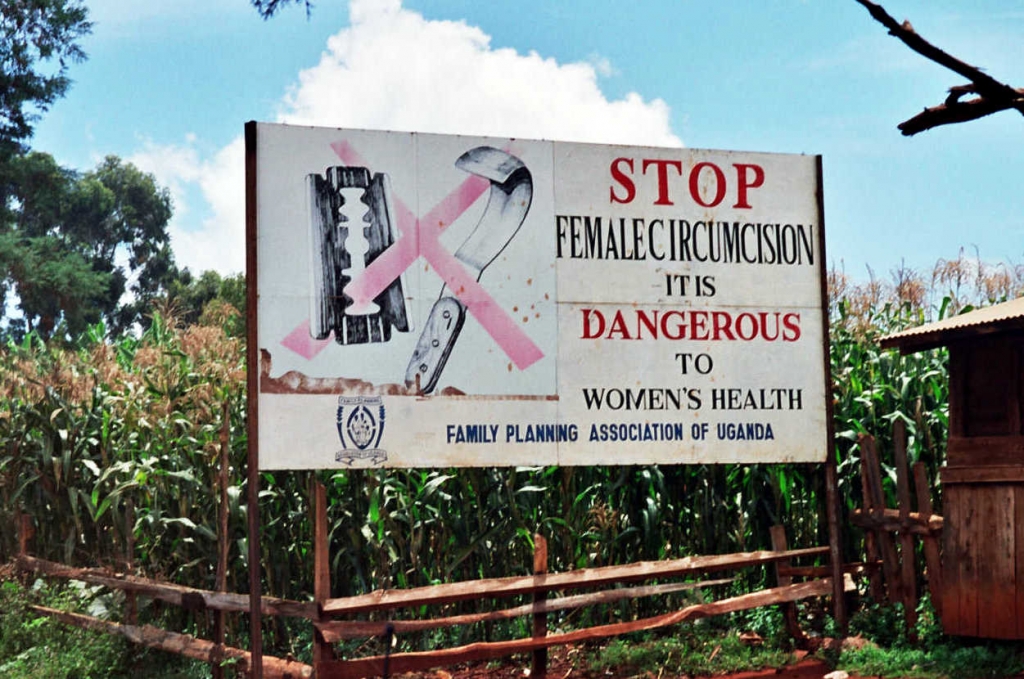
This second part of the interview picks up where Sofia and Dalia left off, rounding off first the topic of appreciating the many differences that exist between contexts, even when these are geographically close together. They then move on to discussing female genital mutilation (FGM) and some of its possible impacts on the people it is carried out on, as well as its urgent global health significance. This background sets the scene for exploring Dalia’s commitment to activism in this field, particularly in seeking to protect the human rights of women in her own country.
Content warning: please be aware that this interview transcript involves a detailed account of what FGM involves, as well as descriptions of some of its consequences on physical and mental health, which could be distressing for some readers.
Sofia: The conversation so far has really made me think about the importance of not automatically grouping together contexts that are foreign to us and assuming that they must be the same. In every context, every country, and even within countries a lot of the time, the situation is really different.
Dalia: Yes, including within the same country. You can have different areas of the country, or different states, which are completely different. I know that to be true, for example, for my country. Sudan is a very culturally rich and diverse country. We have many tribes. We have 18 states. People with different ethnicities exist in Sudan — African, Arab, and a mix of both, as well as indigenous Nubians and others. And many people are Muslims — over 90% of the population (United States Department of State, 2019), though other religions exist, like African traditional religions and Christianity. Further, geographical locations have different tribes, and these can be quite different, in terms of — for example — what they think is ‘OK.’ To illustrate, in the capital city (Khartoum), where a lot of people are working, getting educated, etc., they’re kind of abandoning the child marriage notion. But maybe if you take a bus and go quite far from the centre, you’d realise that somewhere else — in the same country — it is still quite prominent (Elduma, 2018). While people in the big cities or big states are abandoning FGM, you’d see that it is quite common still in other places. There are places that are still very much holding onto these practices.
Sofia: So would you say that it’s an urban-rural divide? Is that a factor, perhaps? Or is a religion-based divide? Or a combination of different elements?
Dalia: I personally think that there is some kind of urban-rural divide, yes. My personal impression is that when people realise what the harms [of child marriage and FGM] are, for example, when they’re outside of their immediate and often rural communities, they question these practices more. For example, when they are in the big cities where people are having more conversations, and maybe getting more educated about the harms of these practices. And then they’re maybe more inclined to abandon them. In fact, for me this was especially noticeable when I was going on ‘medical missions’ in medical school, because often when we would have any campaigns to abandon harmful traditions or practices like FGM, we would target mainly the rural areas. That said, it is still there in the urban areas, it’s not totally eliminated, but overall I think you’re more likely to find these practices in rural areas (Elduma, 2018).
Sofia: I think this is perhaps a good lead into talking about your work in FGM activism. Before we begin, and if you feel comfortable, could you give a brief description, for people who might not know, of what FGM is?
Dalia: FGM, or cutting, is defined as all procedures that involve partial or total removal of the external female genitalia, or any other injury to the female genital organs for non-medical reasons. These procedures are mostly carried out on young girls, often between infancy and adolescence, though occasionally also on adult women. It is recognised as a violation of human rights (World Health Organisation, 2020). And it’s classified into four major types (World Health Organisation, 2020). The first type is the partial or total removal of the clitoral glands, and or the clitoral hood. The second type is the partial or total removal of the clitoral glands and the labia minora, with or without the removal of the labia majora. Type three, which is the one with the highest likelihood of complications, is also known as infibulation. This is the narrowing of the vaginal opening through the creation of a covering seal. The seal is formed by cutting and repositioning the labia minora or the labia majora, sometimes through stitching. The clitoral hood and glands may or may not be removed. Finally, type four is ‘other harmful procedures’, like pricking, piercing or cauterising the genital area, again, all for non-medical purposes. The most common across the world are types one and two, and unfortunately in my country, Sudan, the most common one is the type three (UNFPA, 2020).
Sofia: Could you possibly talk about the Global Health significance of this problem?
Dalia: According to the WHO, over three million girls are estimated to be at risk of having an FGM procedure carried out on them every single year. More than 200 million girls and women alive today have been cut, again according to WHO. This is mostly in 30 countries across Africa, the Middle East and Asia, where cases of FGM are concentrated (World Health Organisation, 2020). And the procedure has absolutely no health benefits for girls and women, instead it subjects them to unnecessary consequences: physically, mentally, and in regards to their sexual health, too (UNFPA, 2020; World Health Organisation, 2020). And sometimes these consequences can become life-long, for many women. So FGM can cause severe bleeding and problems urinating. It can cause cysts and infections. It can also complicate childbirth, and lead to an increased risk of neonatal death. Mentally, it can cause issues like depression, post-traumatic stress disorder and anxiety, and it also affect sexual health. For example, in the form of painful sexual intercourse. It can affect a woman’s life so much that the injury may need to be re-opened, and surgery performed on the woman (World Health Organisation, 2020). And then the other aspect is that girls who do not get an FGM procedure done may be socially excluded or stigmatised in their countries. They may not be able to marry in their community, which can also in turn cause psychological trauma for them as well (Bedri et al., 2019; Omigbodun et al., 2020).
Sofia: Thank you for providing us with a thorough background into this problem, and highlighting why it is such a key Global Health issue. Can you talk to me about your personal activism in this area? Perhaps why you chose this field, as well as what you have done within it?
Dalia: Like I mentioned earlier, it was sort of a coincidence how I found IFMSA’s SCORA and how I started working with them (IFMSA, s. d.). And their biggest project in Sudan — every single year — would be the anti-FGM project (Sudan MedSIN, 2019). That’s how I started working in it. At that time I was a second year medical student, and I didn’t know much about FGM. It’s not really talked about or taught that much, either. It is quite a sensitive issue, and sometimes taboo even. So I really needed that exposure [through SCORA], in order to understand quite how problematic it is. And I was completely shocked. I actually could not believe that I’d had no idea about the harm it causes. And I guess that this kind of drew me to working on this specific project. It was helpful too that there was a lot of support from other organisations for this cause — it really was a focus within activism in Sudan in general.
Sofia: When you say other organisations do you mean non-governmental organisations, or governmental bodies, or something else? Where was the support coming from?
Dalia: A lot of the support was coming from the WHO in Sudan. They used to collaborate with us [SCORA] a lot, and fund a lot of our projects. Every single year we would have a big campaign for our FGM project, around the International Day of Zero Tolerance for FGM, which is on February 6th (United Nations, s. d.). So we would have a whole campaign for about a month. We would have medical missions, as well as social media campaigns, and workshops also for medical, nursing and midwifery students. We would end the month with an event for the International Day. We also had support from, and collaborated with, other local organisations within Sudan, which are specifically working on FGM. And we also worked with the Ministry of Health in Sudan.
Sofia: Could you tell me more about what your campaigns would look like?
Dalia: We would go to people in the market, or at the mall, or if it’s the medical missions in rural regions, we’d gather people in a big space — such as a school, for example. Once there, we would talk to the people present about FGM, and answer their questions as well. Then during the workshops we would try to make healthcare students more aware about FGM, and urge them to support girls and women who’ve received the procedure not only through managing physical complications, but by also building rapport and considering the psychological impact FGM might have on the patient. At the end of the sessions students would often sign a declaration that they would not perform FGM at any time during their practice, — as we are against the medicalisation of FGM — and we actually gathered thousands of such signatures.
Sofia: I’m aware that the process of activism is in and of itself important and impactful, but I’m curious: did you have any big successes or face any particularly memorable challenges?
Dalia: One of the main challenges is that it is a very sensitive topic. So it is often quite hard to get people to actually listen when you’re trying to tell them about the negative aspects of FGM. It carries a lot of weight when you tell a grandmother or mother who has been involved in FGM being carried out on their granddaughter or daughter that this practice is harmful, or that this should be stopped in the future. It’s challenging, even if it’s a message that you feel is important to get across. And sometimes, people do not want to listen, because it’s attached to other things — culturally, for example. And there is a wide misconception that religiously it’s an obligation, which most clerks do not support. But it’s a misconception (Global Citizen, s. d.; World Health Organisation, s. d.). And there’s other misconceptions: that FGM relates to hygiene; that it’s a sign of beauty; or that it decreases the sexual desires of women, such that they might be less likely to have sexual relations before or outside of marriage (Global Citizen, s. d.; World Health Organisation, s. d.). So it’s all of these reasons that have made it this way. In our activism, we tried very hard to show that is not within Islamic religion to require performing FGM. For example, in Sudan we call the third type the ‘Pharaonic’ type, because it is believed to date back to Ancient Egyptian and Nubian times (Elduma, 2018). So we try to make sure that there is an understanding that it is not based in religion, and that this is a misconception. From there it is much easier to convince people to consider abandoning the practice.
Sofia: I guess the thing hearing you that is in my mind is that people have their internal logic, right? They’re not doing this to go out and do harm. It is perhaps worth remembering that people are not doing this to their daughters and granddaughters because they want to harm them.
Dalia: Yes, exactly. And many argue, for example if you talk to many grandmothers, that “well, I’ve had ten children and my daughter has had five, and we’ve never had a problem.” And then you’re trying to say to them, “well, I’m really glad that this did not happen to you, that’s really good, but there’s a chance — because it has no benefit, it is not necessary, and it actually can cause a lot of harm.” But then it is hard to convince them, because it is their lived experience that this is fine. It’s their lived experience that this makes you more desirable, which is good, because it means that your daughter is more likely to get married. And they tell you stories, and when you really listen, you realise that when FGM is done, it’s bad — but also, if it’s not done, from a different perspective it can be really bad also. So sometimes it feels like: which fire do you choose? It’s that ingrained into the social norms that deviating from it is stigmatising. But sticking to it can be harmful. So, which one do you pick? That is I think the biggest challenge: to get people to completely understand that we can together change the social norm, and that this would be something positive.
References:
Bedri, N., Sherfi, H., Rudwan, G., Elhadi, S., Kabiru, C., & Amin, W. (2019). Shifts in FGM/C practice in Sudan: Communities’ perspectives and drivers. BMC Women’s Health, 19(1), 168. https://doi.org/10.1186/s12905-019-0863-6
Elduma, A. H. (2018). Female Genital Mutilation in Sudan. Open Access Macedonian Journal of Medical Sciences, 6(2), 430‑434. https://doi.org/10.3889/oamjms.2018.099
Global Citizen. (s. d.). Debunking 12 Myths About Female Genital Mutilation (FGM). Global Citizen. Consulté 30 septembre 2021, à l’adresse https://www.globalcitizen.org/fr/content/fgm-female-genital-mutilation-misconceptions/
IFMSA. (s. d.). Sexual and Reproductive Health and Rights including HIV and AIDS (SCORA). IFMSA. Consulté 30 septembre 2021, à l’adresse https://ifmsa.org/standing-committees/sexual-reproductive-health-rights-including-hiv-aids/
Omigbodun, O., Bella-Awusah, T., Groleau, D., Abdulmalik, J., Emma-Echiegu, N., Adedokun, B., & Omigbodun, A. (2020). Perceptions of the psychological experiences surrounding female genital mutilation/cutting (FGM/C) among the Izzi in Southeast Nigeria. Transcultural Psychiatry, 57(1), 212‑227. https://doi.org/10.1177/1363461519893141
Sudan MedSIN. (2019). Sudan Anti FGM campaign. IFMSA. https://ifmsa.org/sudan-anti-fgm-campaign/
UNFPA. (2020). Female genital mutilation (FGM) frequently asked questions. https://www.unfpa.org/resources/female-genital-mutilation-fgm-frequently-asked-questions
United Nations. (s. d.). International Day of Zero Tolerance for Female Genital Mutilation. United Nations; United Nations. Consulté 30 septembre 2021, à l’adresse https://www.un.org/en/observances/female-genital-mutilation-day
United States Department of State. (2019). Sudan 2019 International Religious Freedom Report. 15.
World Health Organisation. (s. d.). WHO | Female genital mutilation. WHO; World Health Organization. Consulté 30 septembre 2021, à l’adresse http://www.who.int/reproductivehealth/publications/fgm/FGM_infographics/en/
World Health Organisation. (2020). Female genital mutilation. https://www.who.int/news-room/fact-sheets/detail/female-genital-mutilation
Like what you read?
More from Sofia Weiss Goitiandia here.

