Li L, Barnes M, Aldinger C, Bierer B. Global Clinical trials: ethics, harmonization and commitments to transparency. Harvard Public Health Review. Spring 2015;6. DOI: 10.54111/0001/f2.
Over the last two decades, globalization of clinical trials, particularly those sponsored by global foundation and government funders (e.g., Bill and Melinda Gates Foundation, National Institutes of Health, Wellcome Trust) and multi-national pharmaceutical companies, has steadily increased. This increased globalization of clinical trials has been attributed to multiple factors, including access to well-characterized and often treatment naïve, willing participants, thus expediting enrollment; availability of qualified local investigators who are eager to conduct trials; the enhanced capacity of international sites; and the lower cost of conducting trials in developing countries. Economic incentives to site trials in developing economies also stems from the dramatic increase in clinical trial costs in the United States and Europe–one publication cites a $600M cost savings per year (assuming 60,000 trial participants) through shifting 50 percent of late phase trials from the U.S. and Europe to less costly locales such as India and South America. Indeed, the majority of clinical trials regulated by the United States Food and Drug Administration are now performed in multi-national settings. Further, national regulations increasingly require local, in-country study data to demonstrate that a medicinal product or device is efficacious and safe in that country and thus across racial and ethnic groups. These regulations propel multi-national pharmaceutical companies to consider involving these multi-regional sites early in any drug development program.
Despite the rise in clinical trials globally, the conduct of such trials is particularly challenging in developing countries, for a variety of reasons. Appropriate medical care and the infrastructure for the delivery of health care are not universally available. The relative scarcity of health care resources poses particular challenges especially as prevalence of both communicable (e.g., HIV/AIDS, tuberculosis, and malaria) and non-communicable diseases (e.g., diabetes) tends to be high in developing countries. Comparative effectiveness research, implementation science, and identification of efficient and effective new diagnostic and treatment modalities are needed to address these health issues, but the ability to conduct research studies and clinical trials in these settings is often limited due to undeveloped clinical trial infrastructure. Yet investment in such infrastructure can bring essential professional training, clinical resources and medical treatment to developing countries and localities, and their institutions and patients.
Investment by study sponsors spurs improvement in health care and offers benefits to host countries, including (1) investment in local infrastructure (hospitals, clinics and laboratories), (2) training of clinical investigators, health care providers, and support personnel, (3) improvements in the standard of patient care and expertise, and (4) patient/research participant access to novel medications. The clear benefit of investment must be balanced against key challenges to the design and conduct of global clinical trials in emerging economies. The expansion of trials from high resource regions to developing countries has faced rigorous ethical scrutiny. The specter of exploitation underpins many ethical concerns of trials in developing countries.4 Are patients in developing countries free to decide whether or not to participate in research, if access to essential medicines is tied to research? How can “informed consent” be assessed, risks and benefits understood, when the element of choice is so different among research settings? What is “undue influence” in settings where the cultural norm may anticipate the abrogation of autonomy to another? Should or do cultural norms influence the design and conduct of clinical trials? Can patients in low-resource countries undertake the risks involved in testing new medications and advancing medical science if, despite the availability of the medicine, the community is unlikely to benefit widely for reasons of access or cost thereafter?
The doctrines for ethical conduct of medical research involving human subjects embodied in the Belmont Report, the Declaration of Helsinki, the Council for International Organizations of Medical Sciences (CIOMS) and others form the ethical foundation upon which human subjects research can be appropriately conducted. More recently, Emmanuel et al posited seven key requirements that must be met for clinical research to be considered ethical including: (1) scientific or social value; (2) scientific validity; (3) fair subject selection; (4) favorable risk-benefit ratio; (5) independent review; (6) informed consent; and (7) respect for potential and enrolled subjects of multi-regional clinical trials. These principles are universal, broad, and generally self-evident, and do not depend on sponsor, country, study population or site. It is the application of these principles, however, in the nuanced and specific clinical research situations that requires open discussion and for which many questions remain unanswered. It is only with open dialogue that sponsors, health care providers, government regulators and – most importantly— trial participants and the public will become comfortable that clinical trials are not exploitative but fair, necessary, and often beneficial. Transparency in that debate and dialogue is critical.
Clinical trial protocols invariably invoke “the study will be performed in accordance with the ethical principles invoked in the Declaration of Helsinki” in an “ethics” section. However aside from this standard declaration, the ethical underpinnings of clinical trials are almost never directly addressed in the clinical trial protocol – the process document that determines how a study will be conducted. The typical lack of any explicit consideration of the ethical choices made in the design of a clinical trial makes it difficult for research ethics committees (RECs)/institutional review boards (IRBs), bioethicists, clinicians, regulators and others to discern whether and how the sponsor has effectively addressed relevant questions. The ethical questions and approaches to answer those questions may be embedded in the study design but are rarely explicit or discussed in any written document. Whether the appropriate and focused ethical questions have been addressed at all is therefore often unclear. The problem is aggravated by the fact that members of the clinical research team—,whether industry, non-profit, or academic members serve as the protocol writing team—often lack specific training and guidance to recognize and address relevant ethical issues. This can result in protocols with insufficient ethical analysis. Appropriate training and guidance of reviewers is also, at best, uneven. The pervasive use of protocol templates in many organizations results in the inclusion of vague references to international ethics statements without specific plans and justifications for how ethical issues have been addressed and will be managed in thisparticular protocol.
The Multi-Regional Clinical Trials Center at Harvard University (MRCT Center) is a collaborative effort to improve standards for the design, conduct and oversight of multi-regional clinical trials, with a particular focus on trials sited in the developing world. The MRCT Center ensures that all stakeholders—including patients and patient advocates, academia, industry, clinical research organizations, and regulators—are engaged in the analysis of any problem and creation of practical solutions such as training materials, guidance documents, and tools to enable sponsors of clinical trials (industry, government, non-profits and others) to meet many of these ethical requirements. The MRCT Center, alarmed by the absence of explicit ethical reasoning in many protocols, has sought to address this deficiency.
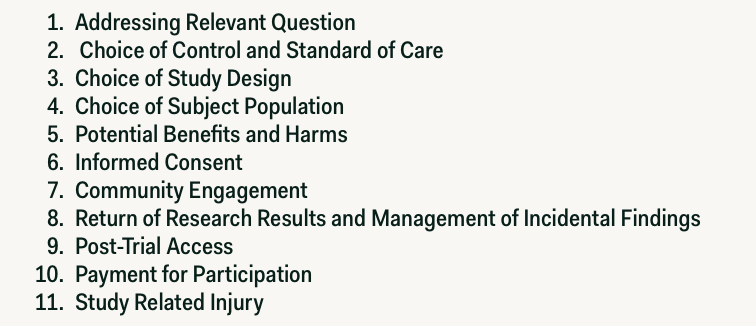
In this context, the MRCT Center convened a multi-stakeholder workgroup to develop tools and guidelines to assist protocol writers in recognizing and addressing common ethical challenges in clinical trials as well as raising the overall quality of clinical trial protocols. This team developed a Protocol Ethics Toolkit that identifies 11 Essential Elements (see Figure 1). This toolkit includes detailed points-to-consider in user-friendly worksheets as well as useful examples that guide users towards drafting a standardized ethics section. The toolkit is not prescriptive; rather, it illuminates central questions, gives examples and considerations, and encourages analytic discourse. Recently, in collaboration with the Global Health Network at Oxford University, this Essential Ethics Toolkit has been transformed into an e-learning resource and has launched as a modular course that is geared toward users in developing countries. The Ethics Tool Kit is also intended to assist ethics committee members who may lack sufficient time or breadth of experience in reviewing complex protocols to analyze clinical trial protocols in a more efficient, comprehensive manner.
These resources recommend that protocol writers address ethical issues through a dedicated ethics section incorporated into all study protocols. This ethics section would address the ethical concerns for a study in every geographic region proposed for siting the study and would require study teams to think through and address ethical considerations prior to ethics committee review. Issues to consider may include effective communication of consent materials, potential conflicts of interest related to inducements to participate (such as access to medical care associated with the clinical trial), and potential cultural differences associated with the ethics committee review process. It would allow for an analysis and explanation of any differences in the conduct of the trial in different locations (e.g., industrial versus developing economies, urban versus rural versus tribal communities). Incorporating this ethics section would ensure that each of the overarching principles of the ethical conduct of research is addressed for this specific trial in this specific region. Importantly, it would allow RECs/IRBs to orient quickly to relevant questions and to ensure that they agree with the ethical choices made. It may be particularly helpful for RECs in developing countries that may lack expertise or resources to review complex protocols, and that may question – but do not know how to answer – whether the protocol under review is identical to or different from the protocol as approved in other countries. For study teams developing protocols and for RECs/IRBs, the Ethics Tool Kit provides a rigorous, comprehensive, and efficient methodology to ensure that ethical issues have been properly considered and addressed. It contributes to making ethical considerations explicit, so that the ethical challenges of multi-national clinical research will be transparent and addressed prior to protocol approval.
The MRCT Center is committed to transparency, open discussion, deliberation and dissemination of common approaches and solutions, standards, tools and guidance. Of course, capacity building, training and resources are essential to ensure the ethical and appropriate conduct of clinical trials, particularly in the emerging economies and the developing world. The MRCT Center and others are developing such resources for widespread dissemination, with the hope that universal adoption (and iterative improvements) will provide a common platform for multi-regional clinical trials. Such initiatives include:
The last factor – international regulatory engagement – deserves particular mention. The more that clinical trial regulations differ from country to country, the more difficult it will be to establish common approaches to current pressing ethical issues. For instance, if the regulatory authority of one country requires participant access to trial medications in all instances (e.g., independent of alternative treatments, sufficient safety data or review) after a trial, while another country does not, is it then fair or ethical for one participant to have access to the drug while another participant in the same trial does not, simply based on his or her place of residence? If one regulatory authority requires compensation for serious adverse events or death related to participation in a clinical trial while another does not, is it then fair or ethical to “value” one life differently than another? Harmonization of the regulations, requirements, and directions will help to ensure that ethical solutions to these issues, even if challenging, are at least feasible.
Globalization of clinical trials will continue; however, only if trial design, conduct and implementation are maintained at a high ethical standard will multi-regional clinical trials be embraced by local communities and the governments of non-OECD countries. Accusations of exploitation and malfeasance will erupt intermittently if public and transparent discourse is not embraced. The development of ethical standards – and performance standards – in multi-regional trials is a process that will evolve effectively only if deliberations are public and transparent, able to be reviewed, debated, and discussed. The integration of ethical principles as outlined above in the development of global clinical trial research—and the open discourse that will result—will help to improve the ethical conduct of such trials, enhance public trust, and preserve the integrity of the science conducted.
Glickman, S. W., McHutchison, J. G., Peterson, E. D., Cairns, C. B., Harrington, R. A., Califf, R. M., and Schulman, K. A. (2009). Ethical and scientific implications of the globalization of clinical research. New England Journal of Medicine, 360(8), 816-823.
Lang, T., and Siribaddana, S. (2012). Clinical trials have gone global: is this a good thing? PLoS Medicine, 9(6), e1001228.
Garnier, J. P. (2008). Rebuilding the R&D engine in big pharma. Harvard Business Review, 86(5), 68-70.
Schuklenk, U. (2010). For-profit clinical trials in developing countries—those troublesome patient benefits. The American Journal of Bioethics, 10(6), 52-54.
National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. (1979). Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research. Washington, DC: U.S. Department of Health and Human Services.
World Medical Association. (2001). World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bulletin of the World Health Organization, 79(4), 373.
Council for International Organizations of Medical Sciences (CIOMS) and World Health Organization. (1993).
See for example: (a) The Nuremberg Code. JAMA. 1996:276:1691; (b) International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). Good clinical practice: consolidated guidance. 62 Federal Register 25692 (1997); (c) European Forum for Good Clinical Practice. Guidelines and Recommendations for European Ethics Committees. Leuven, Belgium: EFGCP; 1997; and (d) Medical Research Council (UK). Guidelines for Good Clinical Practice in Clinical Trials. London, England: MRC; 1998.
Emanuel, E. J., Wendler, D., and Grady, C. (2000). What makes clinical research ethical?. Jama, 283(20), 2701-2711.
The Multi-Regional Clinical Trials Center at Harvard University
MRCT Ethics Essential Elements and Points to Consider Reference Document
Essential Elements of Ethics
MRCT Workshop Meeting Summary, Nov 20, 2011; “Ethics Committee Panel (A. Davis)”
Sonstein, S. A., Seltzer, J., Li, R., Silva, H., Jones, C. T., and Daemen, E. (2014). Moving From Compliance to Competency: A Harmonized Core Competency Framework for the Clinical Research Professional.
Ellenberg, S. S., Fleming, T. R., and DeMets, D. L. (2003). Data monitoring committees in clinical trials: a practical perspective. John Wiley & Sons.
Mello MM, Francer JK, Wilenzick M, Teden P, Bierer BE, Barnes M. (2013). Preparing for responsible sharing of clinical trial data. New Engl J Med. 369:1651-58.
Return of Results MRCT Guidance Document and Return of Results MRCT Toolkit.
Post Trial Access Responsibilities
Rudd, R. E. (2010). Improving Americans’ health literacy. N Engl J Med, 363(24), 2283-5 and US Department of Health and Human Services. (2010). Simply Put: A Guide for Creating Easy to Understand Materials.
Causality Training
Global Regulatory Engagement
Rebecca Li, PhD is the Executive Director of Vivli, the Center for Global Clinical Research Data and on faculty at the Center for Bioethics at the Harvard Medical School and serves as the Co-director of the Research Ethics Program.
Mark Barnes, JD LLM is a partner at Ropes & Gray LLP, a lecturer at Harvard Law School and Visiting Lecturer in Law at Yale Law School. He also serves as Harvard faculty co-chair for the Multi-Regional Clinical Trials Center at Harvard.
Carmen E. Aldinger PhD, MPH is the Senior Administrative and Training Manager at the Multi-Regional Clinical Trials Center, Harvard.
Barbara E. Bierer, MD is the faculty director of the Multi-Regional Clinical Trials Center of Brigham and Women’s Hospital and Harvard (MRCT Center); Professor of Medicine, Harvard Medical School and Brigham and Women’s Hospital, Boston; and a hematologist/oncologist.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()