Kawa N. The Beirut explosion: medical response and resilience. HPHR. 2021;53.10.54111/0001/AAA4
Lebanon is a country that has endured significant political tension since its establishment in 1920. As a result of recurrent conflicts, medical sectors have had to adapt and strengthen their internal capacity for emergency response. All the while, a national disaster plan has yet to be adopted, despite persistent advocacy by experts and physicians. Lack of formal preparedness and chain of command resulted in significant strain of the healthcare sector following the Beirut explosion of August 4th 2020. Since its occurrence, governmental action and accountability have been absent, and the medical sector continues to suffer through the COVID-19 pandemic, and the recent waves of healthcare staff out-migration from Lebanon. Through a series of key informant interviews and a review of available literature, we will explore the historical complexities and governmental shortcomings that impacted the medical response capacities. We will then consider the specific current events, namely the economic crisis and global pandemic, that forced responders into unchartered territories.
Historically, the quality of medical care in Lebanon has often been lauded in the international community, attracting significant medical tourism. Nevertheless, a facet often overlooked is the influence that political turmoil has had on “emergency preparedness training” of healthcare staff. Attending physicians, who continue to practice at the American University of Beirut, reported having to perform life-saving treatments at gunpoint during the 15-year civil war, with limited resources or in the absence of electricity. From a resource planning perspective, many hospitals opted to build their operating rooms underground, to protect from bombings and conflict (Kaafarani et al., 2020). All the while, the country’s long-standing history of power outages resulted in procurement of back-up generators as a standard plan for the routine power supply to the majority of medical centers.
Since the end of the war in 1990, Lebanon’s political and cultural dynamics have not been completely mended. The country has undergone several political assassinations, civilian conflicts, and recurrent instances of mass casualty events (Hitti et al., 2020). In spite of these experiences, Lebanon still lacks a formally structured national disaster management plan. Local physicians and advocates report that political deadlock has stifled all proposals made thus far (El Sayed & Bayram, 2013). In fact, the country does not have an Emergency Medical Technician service or a national blood donation registry. In the absence of a coordinated pre-hospital response system, medical facilities have opted to create their own preparedness plans.
Annex 1: Organization structure of emergency response in Lebanon
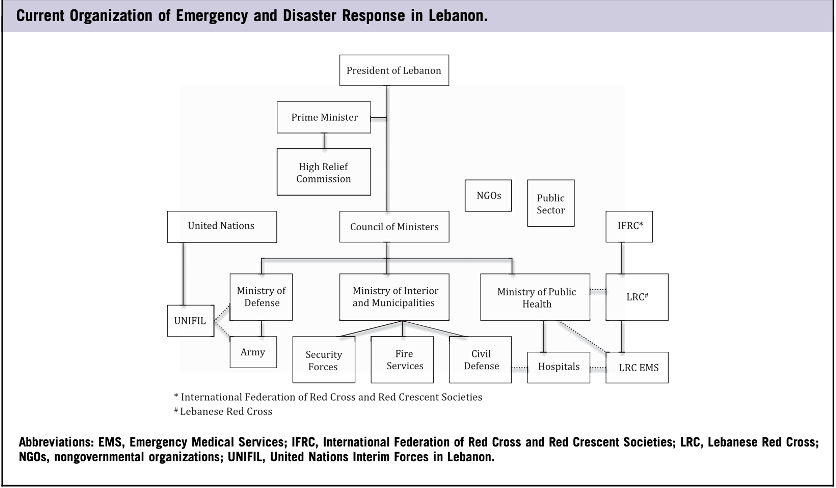
Source: El Sayed, 2013
On a larger scale, the segmented multi-organizational approach to disaster response in Lebanon illustrates its significant complexity (Annex 1). At a national level, emergency response involves the Lebanese army, civil agencies, the Lebanese Red Cross, hospitals, nongovernmental agencies and the public sector. Historically, the army has served as a crucial player in disaster response, in part because it follows a more robust command structure. Nevertheless, the roles, responsibilities, and capacities of the contributing entities are not established, and the chain of command is unclear (El Sayed, 2013). The country also relies heavily on external aid from international agencies such as the United Nations Interim Forces in Lebanon and the World Health Organization. Evaluation of previous emergency responses in Lebanon explicitly state the weaknesses of the system, potential for confusion, system failure, and the need for a more coordinated plan (El Sayed, 2013).
Annex 2: Warehouse 12 location at Beirut Port

Source:BBC news, Available at https://www.bbc.com/news/world-middle-east-53683082
In October 2013, the Rhosus, a Moldova-flagged ship sailing from Georgia to Mozambique, was docked in the Beirut port (Beirut explosion 2020). Disputes surrounding the crew’s unpaid wages resulted in prolonged stationing of the ship, and its contents which were eventually abandoned by their owner, a Russian businessman. The 2,750 tons of ammonium nitrate on board were removed and stored in the port’s warehouse 12 (Annex 2). Over the next several years, at least ten letters were sent to various members of the government and an “urgent matters judge.” These documents reiterated the dangers of storing the highly explosive material in the unequipped facility and requested its immediate disposal (CNBC, 2020). In spite of these pleas, no responses were sent and no actions were taken. After the explosion, Lebanese politicians denied any knowledge of such requests. However, journalists and investigators continue to speak out about the complicated oversight role at the Beirut port, and how all the political parties hold some degree of influence (Kobbesi, 2020).
On August 4th, 2020 at around 6:00 PM, a fire broke out at the Beirut port. It is thought that the source of the fire began in a lot storing fireworks. The port’s general manager noted that welding work was being completed in the warehouse earlier in the day (BBC News, 2020). Witnesses reported hearing several loud sounds and noticing fumes emerging from the port. This lasted for several minutes until 6:07 PM when the fire reached warehouse 12, where the ammonium nitrate from the Rhosus had been stored. A large mushroom cloud erupted which was visible several kilometers away.
Annex 3: Explosions caused by ammonium nitrate- comparative scale
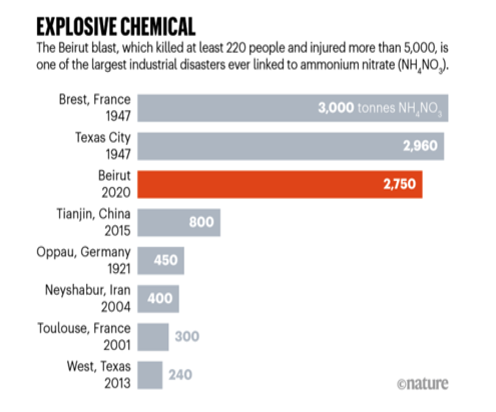
Source: Guglielmi, 2020
Historically, ammonium nitrate has been the culprit responsible for several large-scale disasters. Poorly regulated storage of this hazardous material has resulted in massive explosions in Texas and Tianjin with 240 and 800 tons of ammonium nitrate respectively (Guglielmi, 2020; Annex 3). In Lebanon the 2,750 tons caused large-scale destruction in a 10-kilometer radius, affecting the capital city Beirut, a densely populated area with an estimated 93,855 people per square mile (World’s Capital Cities, 2020).
The timing of the explosion is also an important factor to note. Since August 4th was a Tuesday, many people were on the road returning home after work in Beirut’s usual rush hour traffic. Given the COVID-19 pandemic, few people were out in restaurants and pubs in Gemmayzeh and Mar Mikhael. These highly touristic areas neighbor the port and are generally packed around this time. Nevertheless, even in the absence
Annex 4: Satellite radar imaging of Beirut blast
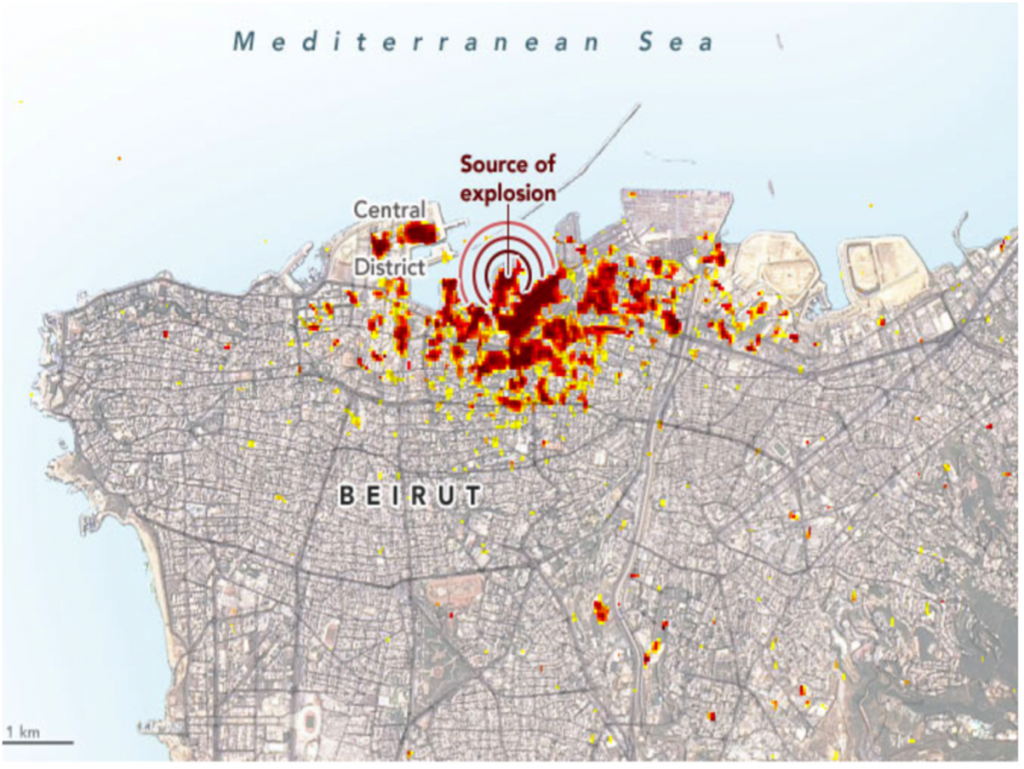
The damage severity follows a color scale ranging from yellow (partial damage) to red (severe damage) with each pixel representing an area of 30 meters by 30 meters
Source: NASA Earth Observatory, available at https://earthobservatory.nasa.gov/images/147098/scientists-map-beirut-blast-damage
Annex 5: Lebanon population density and explosion proximity map
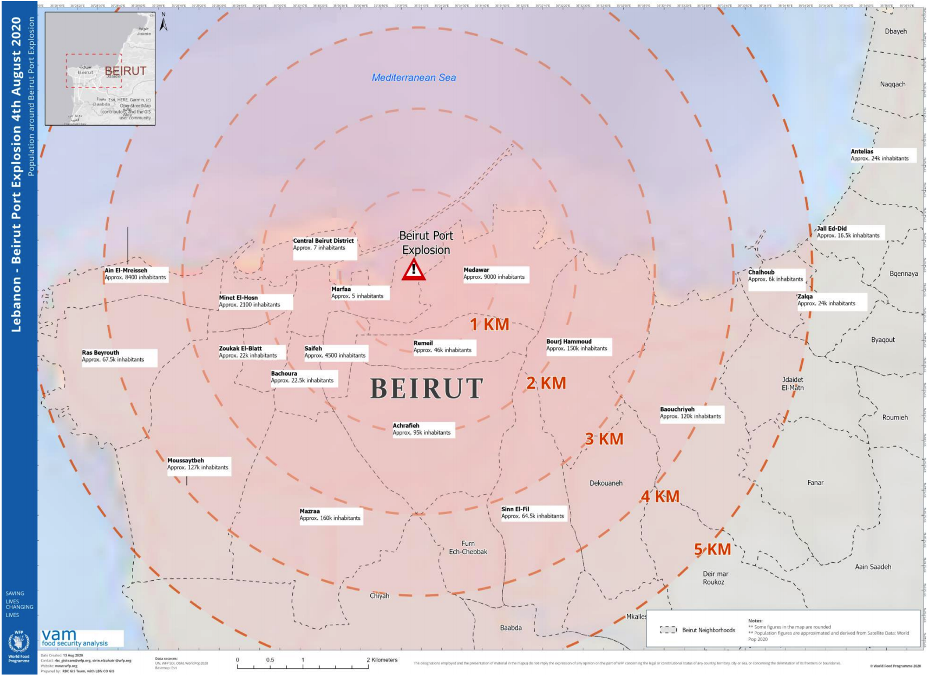
Source: World Food Programme
Available at https://reliefweb.int/sites/reliefweb.int/files/resources/WFP%20Lebanon%20%28Beirut%20Port%20Explosions%29%20Situation%20Report%20%232%2C%2017%20August%202020.pdf
Annex 6: Map Action delineation of vulnerable areas
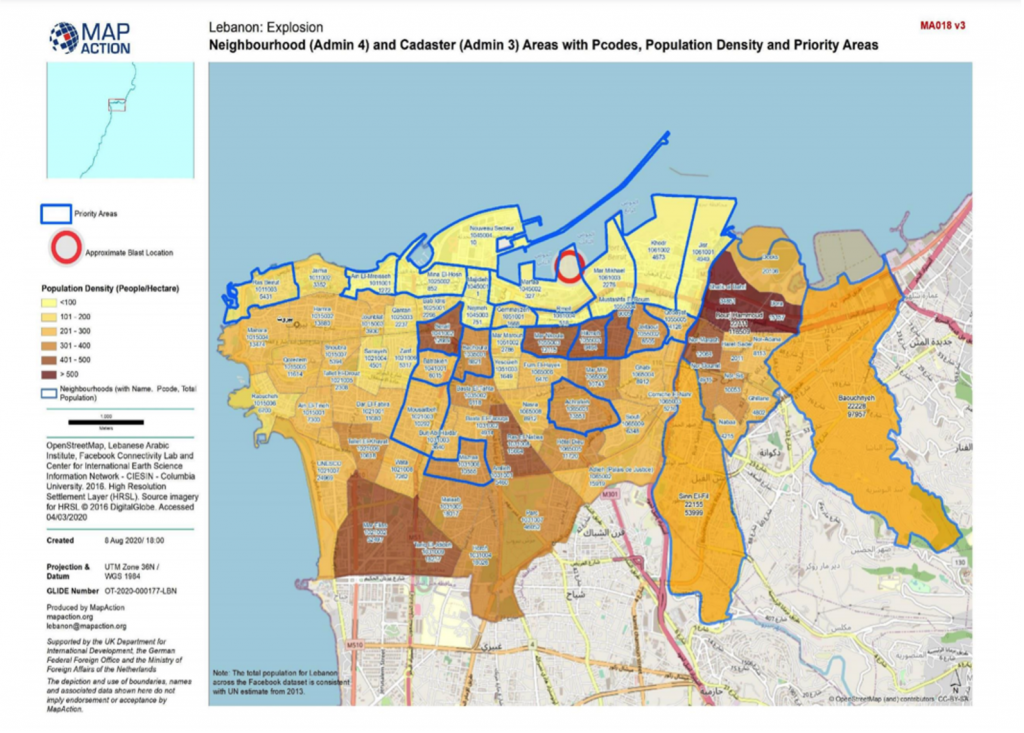
Source: ACAPS secondary data review, available at: https://www.acaps.org/sites/acaps/files/products/files/20200812_acaps_secondary_data_review_beirut_explosion_0.pdf
Several institutions have mapped the extent and severity of the Beirut blast. Satellite radar imaging from the NASA observatory was used to create a damage proxy map comparing the affected area following the blast to days that preceded the explosion (Annex 4). Correlating these findings with population density maps such as those produced by the World Food Programme further depict the gravity of situation (Annex 5). The resulting image depicts not only localized severity, but also scattered affected areas at a distance. ACAPS and MAP Action delineated certain priority areas that are known to be highly populated and , more underserved Annex 6). Bourj Hammoud for example is a predominantly Armenian area that had been in a vulnerable state even before the explosion. It is known for having very narrow streets, poor living conditions and housing upwards of 10,000 Syrian Refugees (acaps, 2020). Following the explosion, the Open Map Lebanon initiative was launched to create a recovery map and continues to serve as an interactive response tool (Open Map Lebanon 2020).
Annex 7: Hospital damage due to the Beirut blast
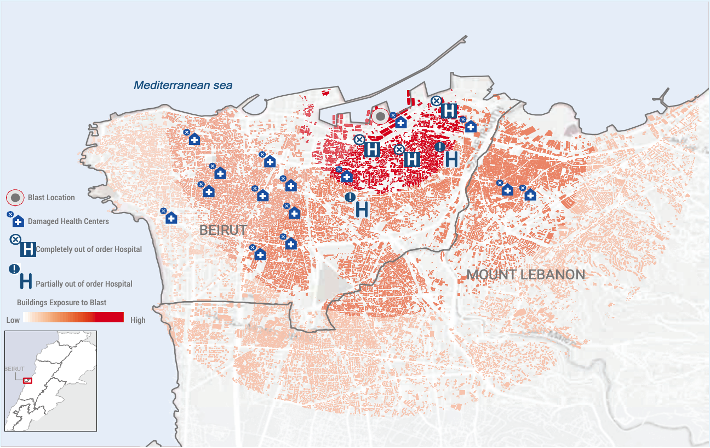
Source: Flash Appeal 2020, available at: https://www.unocha.org/sites/unocha/files/Lebanon%20Flash%20Appeal%20FINAL%2014%20Aug%202020.pdf
Annex 8: Strategy& evaluation of healthcare losses
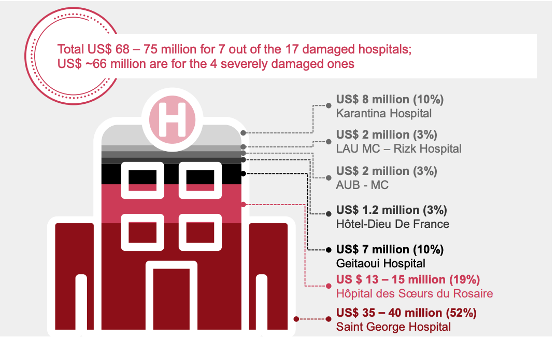
Source: Strategy& Impact assessment, available at: https://www.strategyand.pwc.com/m1/en/beirut-explosion/beirut-explosion-impact-assessment.pdf
In the immediate vicinity of the explosion, 240 buildings underwent severe destruction, affecting 3,210 households (Strategy&, 2020). Further out, an additional 2,570 and 10,610 buildings experienced moderate and mild damage respectively. Overall, 31,000 houses became uninhabitable, leaving roughly 13,000 households in need of shelter. In addition to damages to housing structures, medical centers were also greatly affected (Strategy&, 2020). In the vicinity of the explosion, 17 hospitals and 16 primary healthcare centers were damaged (Strategy&, 2020, Annex 7). In addition, 3 of the affected hospitals (St Georges hospital, Wardieh hospital and Karantina hospital) became completely out of service (United Nations Office for the Coordination of Humanitarian Affairs, 2020). So far, consulting companies such as PwC’s Strategy& have estimated the extent of infrastructural damage to amount to 3.115 billion US dollars of which 75 million pertain to the healthcare sector (Annex 8).
Although the reported numbers vary, it is estimated that approximately 220 individuals were killed in the blast with upwards of 6,500 others injured and in need of immediate care (Cheaito & Al-Hajj, 2020). In the setting of the economic crisis, the hospital system had already been strained. In fact, only weeks before the explosion, one of the country’s largest hospitals was forced to lay off 500 of its administrative and nursing staff (Reuters Staff, 2020). Many other institutions had furloughed employees, leading to significant understaffing at the time of the explosion. All the while, hospital occupancy was already high due to the COVID-19 pandemic.
The large scale of this disaster necessitated widespread medical mobilization. In the absence of a national disaster response, the different entities had to work creatively and collaboratively to fill the needs of those affected. Physicians at certain hospitals reported that there was no official national alert to prompt hospitals about the event and that initial notifications about the explosion came from widespread video footage sent via WhatsApp messaging and news coverage.
Disaster response activities were overseen by the Lebanese Army. Their incident command structure secured the blast perimeter to allow investigation and search and rescue efforts to begin. The primary response was a dual effort between the national Civil Defense (CD) Agency and the Lebanese Red Cross (LRC). The Lebanese CD provides emergency prehospital care and operates the national ambulance service. It is an officially recognized, fire-department based, governmental institution made up of full-time employees and volunteers (El Sayed & Bayram, 2013). The CD operates widely across the nation, but its role is minimal. The LRC is a member of the International Federation of the Red Cross and Red Crescent Societies and is recognized by the state as a public non-profit auxiliary service to the Lebanese army. It provides ambulance and pre-hospital care, blood transfusions, first aid and primary health services. While the LRC plays an extensive role in response to medical emergencies, it is mostly supported by volunteers, and staffs only a small number of full-time employees. The two entities function separately and follow different chains of command (El Sayed & Bayram, 2013). While the CD responds to the Ministry of Interior, the LRC falls under the jurisdiction of the Ministry of Public Health. The LRC coordinates with local hospitals to dispatch patients and has its own set of emergency preparedness drills. Details on the LRC’s response to the blast were provided by Dr. RB, an intensive care anesthesiologist, advisor to the LRC president and volunteer member was interviewed.
Shortly after the explosion, the LRC activated its emergency response plan and contacted the volunteers to mobilize at the site of the explosion. Given the timing of the event, many volunteers were leaving work or on the road. The extensive infrastructural damage led to difficulty in rapid arrival to the scene and rendered the proximal areas unfit for setting up a field hospital as per normal protocol. The unknown nature of the explosive material led to significant concern about entering the epicenter. Although there were concerns about radiation and hazardous material exposure, the medical response sector did not have the luxury of mobilizing respirators or Geiger counters. As a safety precaution, the base camp was set up 2 kilometers away from the blast site. One team performed initial triage on the scene, dispatching the injured either to the base camp for further stabilization, evaluation, and in urgent cases, transfer to nearby hospitals or to distant hospitals if the conditions allowed. Pregnant women with contractions or people with fractured limbs, for instance, were transferred to hospitals in the north and south of the country, up to 3 hours away. This was an unusual response given that the LRC’s protocol normally only mobilizes hospitals within a 5–10-kilometer radius. The dispatch teams needed to coordinate rapid communication with the hospitals to determine capacity and avoid overcrowding. This event required much broader intervention whereby all hospitals in the country worked in solidarity to receive patients. In spite of the efforts to structure the response, the system was severely overwhelmed. Generally, the LRC brings injured patients to the closest hospital and only calls for coordination for transfer between hospitals (El Sayed, 2013). Difficulties in early communication resulted in the LRC dispatching some patients to hospitals that were out of service.
Annex 9: Civilian response- photos shared on social media account “LiveLoveLebanon”

In contrast to the LRC and Civil Defense’s triage on site plan, the civilian response was quite different. In keeping with the local traditions of unity and camaraderie, those who were not injured rushed to the scene or to their injured neighbors, adopting a “scoop and run” approach (Annex 9). While this was a well-intentioned effort, the lack of strategic coordination hindered the triage and dispatch activities described above. In certain instances, injured civilians were walking to nearby hospitals that had also suffered significant damage. In a webinar hosted by Johns Hopkins Center for Global Emergency Care (Razzak et al., 2020), the St. George Hospital ED coordinator Dr. Asmar noted that they had to turn away many injured people as they simply were no longer equipped to function. Dr. Boulos also noted that in the moment, people were behaving with “bounded rationality,” insisting on entering the hospitals to find loved ones or demanding that the injured person they accompanied be prioritized. This created yet another hurdle for the hospital system, especially given that social distancing and use of masks was not always being observed.
The three out-of-service hospitals resulted in a loss of approximately 500 beds and created additional complexity whereby both immediate care and patient transfer needed to be addressed (El Sayed, 2020). In terms of damage, the St. George Hospital experienced the greatest losses, requiring 52% of the healthcare related financial repairs listed above. This tertiary care center contains 7 wards over 9 floors with over 350 beds. In the acute setting their experience was particularly difficult. As of yet, no detailed situation report has been published. For further insight, I interviewed Dr. Fares, an ED attending physician who was on call the day of the explosion. Dr. Fares prefaced his report to me by stating that despite the hospital’s existing disaster plan, the extent of the damage rendered any plan irrelevant. He stated “It was an absolute nightmare. I have worked through multiple mass casualty experiences, but nothing like this. Nothing can prepare you for this.”
Annex 10: Pictures of St. George Hospital before and after the blast
Footage shared by physicians at the hospital on social media

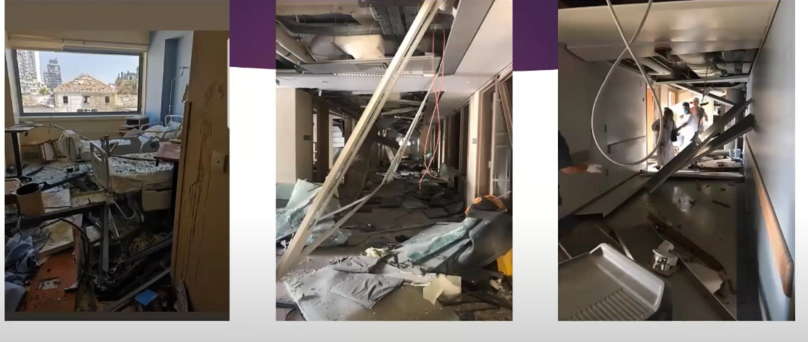

Within seconds of the explosion, there was extensive damage to the St. George Hospital building, loss of electricity and oxygen (Annex 10). The back-up generators serving the ICU remained functional during the next hour. However fears of a power surge resulted in the decision to stop them as soon as possible. At the site of the hospital, 17 perished immediately, including 4 nurses and 13 patients and visitors. Among the staff, patients and visitors, there were upwards of a 100 injured. Within the first few minutes after the blast, hospital house staff began arriving at the ED. Evacuation plans as well as casualty triage efforts began shortly after. Two parking lot areas staffed by resident physicians were designated as the “green zone” where wound cleaning and suturing took place. The ED driveway was split into “yellow and red zones” for more severe injuries, intubation and resuscitation efforts. During this time, all elevators were out of service and over 200 patients were carried down the stairs. They were evaluated and triaged into the different zones while awaiting transfer. The COVID unit holding 16 patients was the last to be evacuated in attempts to reduce exposure. Major challenges described included inability to access medication and supply storages that were also damaged; inability to monitor patients due to destruction of machines; and inability to take adequate COVID precautions. Transfers to nearby hospitals were coordinated by the Emergency Department (ED) Nurse Manager Mr. Saad, the hospital Chief of Staff, and LRC.
Annex 11:Summary data from 3 large hospitals
Hospital | AUBMC | LAUMC-RH | HDF | total |
Treated | > 270 treated in ED | > 400 | 138 treated in ED > 200 on ED sidewalk | > 1,138 |
Admitted | 108 | 72 | 97 |
|
Surgeries on day 1 | 17 | 58 | 69 |
|
Declared dead in ED | 9 | 5 | 13 |
|
Data summarized from webinars presented by these institutions
Annex 12: Securing the entrances of AUBMC
Source: photos shared on social media

Annex 13: HDF example of zoning triage
Source: Beirut blast: The emergency response [Zoom Webinar].
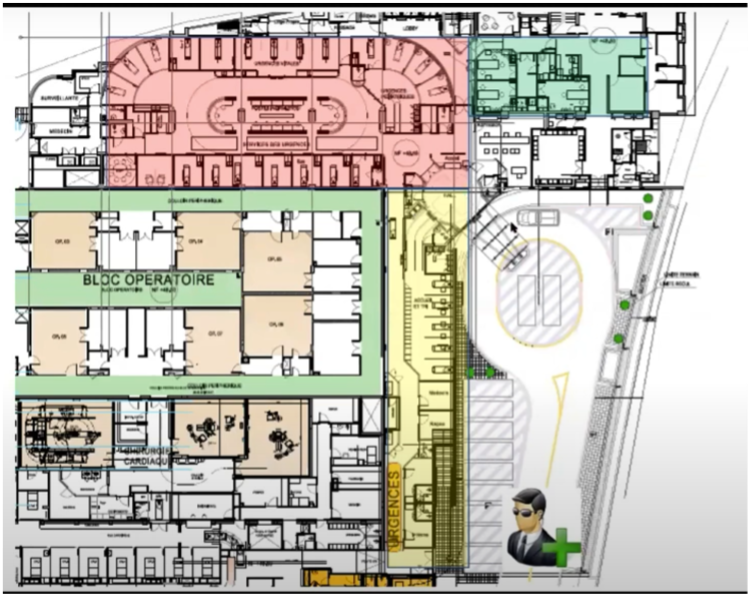
| Zone | Activity |
Green
| Patients who could walk and talk and had no injuries to the head, neck or torso. This zone was used for wound cleaning and suturing. Due to the high influx, the green zone was extended into hallways and additional free space |
| Yellow | Casualties with high risk of crashing who needed constant monitoring and re-assessment |
| Red | Critical patients in need of intubation, invasive interventions and resuscitation. The designated area was within the standard trauma bay. |
Further away, large university hospitals that had not been as severely damaged began receiving a high influx of patients. The American University of Beirut Medical Center (AUBMC), the Lebanese American University Medical Center- Rizk Hospital (LAUMC-RH) and the Hotel Dieu de France (HDF) are three such examples. Based on numbers reported in the webinars, these institutions only treated 1/6th of affected individuals (Annex 11). In response to their activation plans, three major domains were called upon: human resources, material resources and space. Standby physicians provided staffing reinforcement and medical supplies were brought to the ED floor. From previous experiences, lockdown of the EDs was noted as another essential step to avoid crowding or stampedes. This necessitated both human and physical barriers to secure the entrances (Annex 12). As mentioned above, the highly emotional response of civilians might have hindered the hospital activities. Only those identified as needing treatment were allowed to enter. Otherwise, triage was conducted in the surge area outside the hospital and was run by a senior level nurse at AUMBC and an ED attending physician at LAUMC. This was done in anticipation of an “upside-down triage” whereby the walking wounded would likely arrive early on and saturate the system (Hitti, 2020). In addition, the HDF response also incorporated a biomedical engineering team that was tasked with ensuring functionality of medical equipment. Once again, color-coded zones were used to separate patients according to severity, this time inside the hospital (Annex 13).
The preparedness plan at AUBMC entails tiered activation whereby an initial alert status precedes the full activation as described by the Chair of the ED, (Razzak et al., 2020). The hospital’s emergency preparedness plan relied on the ED as the point of activation. This was done by a WiFi messaging system given its historical reliability (WhatsApp). Other forms of telephone message alert communication were used for redundancy, although these were later noted to have experienced delays. The hospital received nearly 400 patients and their arrival was described as three consecutive waves (Plaster, 2020). The first one, consisting of those with minor injuries, arrived within the first 15 minutes. The second one followed nearly 40 minutes after the explosion, peaking within the hour and a half following the event and only beginning to attenuate at approximately hour three when the third wave arrived. This consisted of the more severe crush injuries, those extricated from the rubble and those who were dead on arrival.
The LAUMC, a private hospital 2.8 kilometers away from the blast, was one of the few hospitals in the Ashrafiyeh area that was still receiving victims. Although the institution does have its own preparedness plan, they experienced additional complexity due to the fact that their ED was under renovation. A disaster plan for the temporary department had been written however no drills had ever been run. Rapid adaptation was needed in order to restructure the plan in a way that could fit the needs at the time. This need resulted in a delay in activation. Dr. Tanios noted that “the ED rapidly exceeded full capacity before we could initiate our disaster plan” (Razzak, 2020).
Annex 14: Mass mobilization of health professionals
Source: photos shared on social media and news outlets



The HDF hospital, having already reached 70% capacity prior to the explosion, immediately activated “surge capacity response” (Tilsed et al., 2020). They proceeded to open the day hospital and all ambulatory facilities. Unlike the two previous institutions, HDF’s building structure allows for more distance between the hospital gates and the ED entrance. This layout allowed more regulated entry of ambulances and structured triage before entry into the main hospital (Annex 14). Identification cards with serial numbers were filled by hand for every triaged patient, indicating area of injury, vital signs and other noteworthy characteristics. Activities were coordinated in a designated “crisis room.” While the process was well designed, Chief Medical Officer Dr.Dabar explained that with limited human resources, only so much could be done to accommodate the injured. He stated: “Unfortunately, at one point, we had to close the door of the hospital” (Tilsed, 2020).
In spite of the efforts to adequately manage the situation and follow prior plans, certain challenges were evident. The magnitude of patient influx made patient tracking and record keeping extremely difficult. At AUBMC, the electronic medical record system “Epic” was not functional immediately after the blast and required some time to reboot. Prior to switching to the electronic system, the hospital used to rely on manual note taking and tracking, a technique they had since abandoned given the success of “Epic” in previous instances of disaster plan activation. Not having enough paper charts to support caseload, Dr. Hoballah, chair of the department of Surgery noted that they had to resort to “human record keeping” whereby students were assigned to the patients for tracking (Kaafarani et al., 2020). This experience further emphasized the need for redundancy, especially as processes become more technology dependent. In an interview, the former chair of the department, Dr. Kazzi, reported difficulty in communication and staff recognition associated with use of personal protective equipment, an additional burden imposed by the concurrent pandemic.
Private hospitals in the vicinity also responded to the best of their capacity. Dr. RB noted that at Clemenceau Medical Center, patients with superficial wounds were treated with staples, given a Tetanus vaccine and prescriptions for antibiotics before immediate discharge. “We had no options. We had to make room for the more injured” she explained. Dr. Boulos also highlighted the difficulties in receiving adequate patient medical history prior to treatment. She recounted the loss of a young patient with a history of a chronic cardiac condition who was brought to the operating room for treatment of abdominal lacerations. “When we can’t know what we’re dealing with, there is absolutely no way to prepare,” she added. Similar cases were reported by other physicians who were unable to determine critical factors that would normally impact clinical care such as their patients’ use of anticoagulants or medication allergies.
Further away, a number of hospitals also provided substantial support. Located 6 kilometers from the blast site, Rafik Hariri University Hospital, the largest public hospital in the country, had been at the forefront of the COVID response. In partnership with the International Committee of the Red Cross, they also partook in the disaster management. In a series of interviews, Chief Executive Officer Dr. Abiad stated that the hospital received hundreds of patients that night (Meyers, 2020). He added that hospital resources were already quite low prior to the event and that reserves were dwindling. When asked what kind of support would be beneficial, he answered “Anything” (John et al., 2020).
Medical supply shortage was particularly problematic. In the setting of COVID-19 and the economic crisis, medical centers had already been rationing equipment. Physicians at the American University of Beirut noted that in the first six hours following the explosion, they had already used up a year and a half worth of supplies (El Deeb, 2020). In addition, both the Ministry of Public Health’s central warehouse and a recent shipment of personal protective equipment had been stored at the Beirut port and were destroyed (World Health Organization, WHO Iran Update 2020). A vaccine and medication storage facility in the Karantina area was also significantly damaged (ACTED Lebanon, 2020).
Source: ACAPS, 2020
Available at: https://www.acaps.org/sites/acaps/files/products/files/20200812_acaps_secondary_data_review_beirut_explosion_0.pdf
On a more individual note, medical service providers from all levels of training expressed a feeling of duty to serve the injured. Dr. Hoballah noted that staff members who had been let go in the weeks preceding the explosion returned to AUBMC to provide support (Kaafarani, 2020). Residents and medical students, many of whom were also injured, rushed to their respective hospitals to care for patients. Nurses and doctors performed procedures in the dark, using telephones for lighting. Dr. Fares recounted the story of one of the urology residents at St. George Hospital who continued to treat patients before collapsing from a pneumothorax. At the same institution, photos of a nurse carrying three infants made headlines, as she rushed to save them in the midst of the hospital collapse (Annex 15).
Although the initial medical response took place within the first several hours following the explosion, persistent efforts continued for several weeks. Recognizing the need for additional support, local nongovernmental organizations working in healthcare also intervened. In the absence of a national blood bank, Donner Sang Compter, a Lebanese NGO that connects patients with a registered donors mobilized their blood donor database and provided hospitals with needed blood products. In the following days, mobile clinics staffed by volunteers were deployed to help clean wounds and check on patients who had been discharged. Efforts were also made to collaborate directly with the damaged hospitals on a need’s basis.
Early pleas for international support resulted in rapid mobilization of medical teams and experts in casualty extraction. Within the next two days, the country received an influx of providers from Morocco, Switzerland, Italy, Russia, Qatar, Poland, Greece and France among others. Some teams worked in field hospitals built 1 kilometer from the blast site while others focused on rebuilding essential services in damaged hospitals (United Nations Audiovisual Library, 2020). They provided staff assistance, medications and supplies. Language and communication barriers were noted by some of these teams. Lack of clear understanding of the needs was another challenge described (El Sayed, 2020). Private international associations such as Medecins Sans Frontieres also acted rapidly. In addition to providing emergency care, they extended support to continuity care and mental health services (Medecins Sans Frontieres, 2020). They initiated their activities with a needs assessment, going door to door in affected communities and speaking directly with civilians. They identified needs that had previously been neglected such as supply of clean water and hygiene kits.
Even after initial salvage and treatment of the explosion’s victims was complete, hospitals were faced with a new wave of injuries in the days following the explosion. In response to the widespread destruction, large scale volunteering efforts were made to clean the streets and evacuate damaged homes. These dangerous activities caused additional trauma from shards of glass and metal. National outrage surrounding governmental negligence with the explosive material resulted in renewed civil unrest. On August 8th, protestors took to the streets demanding justice, but the situation rapidly escalated when clashes erupted between demonstrators and police forces (Rasmussen et al., 2020). Exchanges of teargas, firecrackers, rubber bullets and stones injured over 170 people who, once again, turned to the hospitals for additional care (Al Jazeera, 2020).
Environmental exposures associated with the blast created an additional concern. Fumes from the ammonium nitrate explosion remained visible in the sky for several hours. Dr. Najat Saliba, an analytical chemist at the Nature Conservation Center at the American University of Beirut expressed her concerns about inhalation injuries and exacerbation of pulmonary conditions in the short run, and long-term consequences of carcinogen exposure (Bollag, 2020). She added that the waste generated from dust, glass powder, pollution and chemicals created a blanket of dangerous material covering most exposed surfaces (Beirut blast may have left 2020). Experts warned that cleaning efforts could create further health risks and urged civilians to take additional precautions (Schuster, 2020).
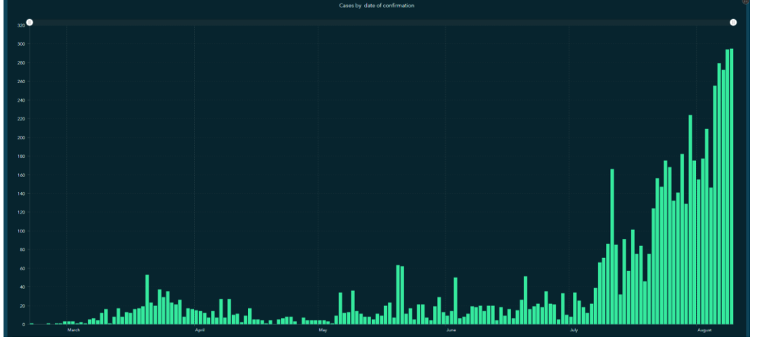
The first case of COVID-19 was detected in Lebanon on February 21st and prompted immediate formation of a National Committee for COVID. On the eve preceding the explosion, a total of 4,022 cases were registered and hospitals had already begun expressing concerns about equipment shortages (Republic of Lebanon Ministry of Public Health, 2020). Some institutions had reported that their ICUs were already at capacity and that they would be unable to receive new patients (acaps, 2020). The emergency response to the Beirut blast upended all mitigation strategies (Berger, 2020). Frontline staff reported that they tried their best to follow recommended guidelines for personal protective equipment when possible. Nevertheless, precaution practices were compromised as physical distancing and COVID screening were simply not possible (El Sayed, 2020). Even after the immediate response, large protests and extensive exposures created another opportunity for COVID transmission (Coles, 2020). Finally, the destruction of homes created a need for densely packed cohabitation (World Health Organization, WHO situation report 2020), further increasing infection risk. In the month following the explosion, the number of COVID cases surged significantly, with a 220 percent increase since August 4th, adding an additional burden to a system on the brink of collapse (International Rescue Committee, 2020, Annex 16).
In addition to the physical and structural toll imposed by the explosion, the negative effects on mental health were devastating. Even before the blast, citizens were experiencing significant emotional hardships due to the economic situation (MEE Staff, 2020). Medical practitioners, nongovernmental organizations, and international aid corporations recognized the growing need for support services, warning about an impending mental health crisis. Local groups such as Embrace and IDRAAC continued to provide a hotline for those in need and noted a significant uptake of this service in comparison to previous months (Jalabi & Georgy, 2020). Many people began exhibiting signs of trauma including nightmares, flashbacks, fatigue and panic attacks (Reuters, 2020). Providers also expressed severe hardships and reduced morale related to implementation of crisis standards of care during the immediate response. In an interview, Dr. Hitti noted the importance of a group debrief session conducted at AUBMC to allow frontline workers to find support among colleagues (Razzak et al, 2020).
Faced with extreme hardships and lack of faith in the potential for prosperity, countless physicians opted to leave the country. The head of the Doctors Syndicate confirmed that, between July and September 2020, upwards of 300 doctors decided to emigrate (Lewis, 2020). In an interview, a former pathologist at AUBMC described the movement as a “mass exodus” and stated, “If I had hope I would have stayed but I have no hope – not in the near nor in the intermediate future – for Lebanon” (Nakhoul & Abdallah, 2020). The Minister of Health Hamad Hassan expressed concerns about the impact this efflux will have on the Lebanese health system, claiming that it will take several years to restore the medical sector after the loss of so many skilled expert providers (Nakhoul & Abdallah, 2020).
Blatant disregard for the safety and wellbeing of citizens resulted in one of the most devastating man-made disasters in recent history. Longstanding governmental negligence and reluctance to structure a robust preparedness plan not only created the perfect catastrophe, but also hindered any chances for a successful response. Lack of coordination and clarity in the chain of command forced institutions to function in isolation from one another. While previous experiences with mass casualty traumas “prepared” hospitals for emergency response, the magnitude of the Beirut explosion was beyond what drills could cover. Unexpected experiences such as severe infrastructural damage, failure of electronic record systems, and renovations in an emergency department reinforced the importance of redundancy in the preparedness plan. The additional burden of an economic crisis compounded with a global pandemic expanded the scope of the explosion’s effects.
The long-term impact on health, livelihood, and excess mortality remains unclear. Factors such as loss of continuity of care, increased exposure to harmful chemicals, increased potential for COVID infection, displacement, and mental health trauma will undoubtedly affect the Lebanese people for years to come. Losses to medical infrastructure and physician reluctance to stay in Lebanon will surely impact the quality of care that can be provided. Lebanese physicians have already begun compiling the “lessons learned” from this experience, but no individual changes on an institutional level can make up for the absence of essential support expected from a functional government.
acaps. (2020, August 12). Emergency operations Centre Beirut assessment & analysis cell: Analysis of affected areas in Greater Beirut. https://www.acaps.org/sites/acaps/files/products/files/20200812_acaps_secondary_data_review_beirut_explosion_0.pdf
ACTED Lebanon. (2020). (rep.). Beirut blast rapid needs assessment report: Karm el Zeytoun, Karantina, Bourj Hammoud, Geitawi & Nabaa neighborhoods. Retrieved from https://www.acted.org/wp-content/uploads/2018/01/lebanon-beirut-blast-rapid-needs-assessment-report-august-2020-finalv2.pdf
Al Jazeera. (2020, August 9). Furious Lebanese plan new protests over Beirut blast. Beirut explosion News | Al Jazeera. https://www.aljazeera.com/news/2020/8/9/furious-lebanese-plan-new-protests-over-beirut-blast
BBC News. (2020, August 11). Beirut explosion: What we know so far. Retrieved December 12, 2020, from https://www.bbc.com/news/world-middle-east-53668493
Beirut blast may have left blanket of hazardous dust over city, says expert. (2020, August 7). The National. https://www.thenationalnews.com/world/mena/beirut-blast-may-have-left-blanket-of-hazardous-dust-over-city-says-expert-1.1060148
Beirut explosion: Tracing the timeline of the disaster. (2020, October 21). ShipTechnology. Retrieved December 15, 2020, from https://www.ship-technology.com/features/beirut-explosion-timeline/
Berger, M. (2020, August 6). After Beirut blast, the race to save lives outweighs coronavirus safety. The Washington Post. https://www.washingtonpost.com/world/2020/08/06/after-beirut-blasts-race-save-lives-outweighs-coronavirus-safety/
Bollag, B. (2020, August 28). Dust left by Beirut’s massive explosion may be a major danger to health. Al-Fanar Media. https://www.al-fanarmedia.org/2020/08/dust-left-by-beiruts-massive-explosion-may-be-a-major-danger-to-health/
Cheaito, M. A., & Al-Hajj, S. (2020, October 18). A brief report on the Beirut Port explosion. Mediterranean Journal of Emergency Medicine & Acute Care. https://escholarship.org/uc/item/6zn9z1j9
CNBC. (2020, August 07). Officials long warned of explosive chemicals at Beirut port. Retrieved December 12, 2020, from https://www.cnbc.com/2020/08/08/officials-long-warned-of-explosive-chemicals-at-beirut-port.html
Coles, I. (2020, August 17). After Beirut explosion, Lebanon faces surge in coronavirus cases. The Wall Street Journal. https://www.wsj.com/articles/after-beirut-explosion-lebanon-faces-surge-in-coronavirus-cases-11597697343
El Sayed, M. (2013). Emergency response to mass casualty incidents in Lebanon. Disaster Medicine and Public Health Preparedness, 7(4), 433-438. https://doi.org/10.1017/dmp.2013.48
El Sayed, M. (2020). Beirut ammonium nitrate explosion: A man-made disaster in times of COVID19 pandemic. Disaster Medicine and Public Health Preparedness, 1-18. https://doi.org/10.1017/dmp.2020.451
El Sayed, M., & Bayram, J. (2013). Prehospital emergency medical services in Lebanon: Overview and prospects. Prehospital and Disaster Medicine, 28(2), 163-165. https://doi.org/10.1017/S1049023X12001732
Guglielmi, G. (2020). Why Beirut’s ammonium nitrate blast was so devastating. Nature news.
https://www.nature.com/articles/d41586-020-02361-x
Hitti, E. A., El Sayed, M. J., Cheaito, M. A., Kellermann, A. L., & Kazzi, A. A. (2020, January 1). Mass casualty management in the emergency department – Lessons learned in Beirut, Lebanon – Part I. Mediterranean Journal of Emergency Medicine & Acute Care. https://escholarship.org/uc/item/742605wb
International Rescue Committee. (2020, September 1). COVID-19 cases increase 220% in month since Beirut explosion – Lebanon. ReliefWeb. https://reliefweb.int/report/lebanon/covid-19-cases-increase-220-month-beirut-explosion
Jalabi, R., & Georgy, M. (2020, August 24). Nightmares, flashbacks, fatigue: Beirut faces mental health crisis after blast. Reuters. https://www.reuters.com/article/us-lebanon-security-blast-mentalhealth/nightmares-flashbacks-fatigue-beirut-faces-mental-health-crisis-after-blast-idUSKBN25K0T7
John, T., Macaya, M., Hayes, M., Renton, A., Rahim, Z., & Upright, E. (2020, August 6). This Beirut hospital may run out of medical supplies soon. CNN. Retrieved December 18, 2020, from https://www.cnn.com/middleeast/live-news/lebanon-beirut-explosion-live-updates-dle-intl/h_869aa3ccc501d09e2fecafdd09bc4b98
Kaafarani, H., Hoballah, J., Safadi, B., Juvelekian, G., & Bulger, E. (2020, September 24). Mass casualty trauma management: Early lessons from Beirut [Webinar]. American College of Surgeons. https://www.facs.org/international/webinar/mass-casualty-management
Khoury, P., Azar, E., & Hitti, E. (2020, August 11). COVID-19 response in Lebanon-Experiences and challenges in a low-resource setting. JAMA. https://doi.org/10.1001/jama.2020.12695
Kobeisi, R., (2020, August 9). رياض قبيسي يكشف تفاصيل جديدة فائقة الأهمية وأسماء بعض المعنيّين بما حدث في مرفأ بيروت. YouTube.
https://www.youtube.com/watch?v=vb1W1qSRqAs&feature=youtu.be
Landry, M. D., Alameddine, M., Jesus, T. S., Sassine, S., Koueik, E., & Raman, S. R. (2020, November 12). The 2020 blast in the Port of Beirut: Can the Lebanese health system “build back better”? BMC Health Services Research. https://doi.org/10.1186/s12913-020-05906-y
Lewis, E. (2020, September 14). Lebanon hospitals under threat as doctors and nurses emigrate. The National. https://www.thenationalnews.com/world/mena/lebanon-hospitals-under-threat-as-doctors-and-nurses-emigrate-1.1077418
Maltesar. (2020, August 12). Beirut explosion: Mental health of people affected is under threat – Lebanon. ReliefWeb. https://reliefweb.int/report/lebanon/beirut-explosion-mental-health-people-affected-under-threat
Medecins Sans Frontieres. (2020, December 3). Lebanon: MSF provides medical and mental health support to Beirut’s most affected communities. Médecins Sans Frontières (MSF) International. https://www.msf.org/lebanon-msf%E2%80%99s-emergency-response-beirut
Meyers, T. (2020, October 13). The Beirut blast left Lebanon’s health system badly shaken. Direct Relief. https://www.directrelief.org/2020/10/the-beirut-blast-left-lebanons-health-system-badly-shaken/
Nakhoul, S., & Abdallah, I. (2020, November 12). Hundreds of disillusioned doctors leave Lebanon, in blow to healthcare. Reuters. https://www.reuters.com/article/us-lebanon-crisis-healthcare-insight/hundreds-of-disillusioned-doctors-leave-lebanon-in-blow-to-healthcare-idUSKBN27S14W
Open Map Lebanon. (2020). https://openmaplebanon.org/
Plaster, L. (2020, September 1). The Beirut blast – Reflections of an emergency physician. Emergency Physicians International. https://www.epijournal.com/home/2020/9/1/the-beirut-blast-reflections-of-an-emergency-physician
Rasmussen, S. E., Osseiran, N., & Nissenbaum, D. (2020, August 8). Clashes erupt in Beirut over deadly explosion. The Wall Street Journal. https://www.wsj.com/articles/beirut-braces-for-mass-protests-over-deadly-explosion-11596883122
Razzak, J., Bayram, J., Asmar, R., Hitti, E., Kazzi, A., & Tanios, A. (2020, November 23). Beirut blast: The emergency response [Zoom Webinar]. Retrieved December 18, 2020, from https://us02web.zoom.us/rec/play/a4iE83rdy_mJJHMBgTSVh6d8Wbai9zNh_TKURvk7tCIfUnzPTbs65l8XUm05678TvUraSgalSJPxs3pO.2ngimPt2KEeK58t9
Republic of Lebanon Ministry of Public Health, Novel coronavirus 2019 (2020). https://www.moph.gov.lb/en/Pages/2/24870/novel-coronavirus-2019-
Reuters. (2020, August 24). Nightmares, flashbacks, fatigue: Beirut faces mental health crisis after blast. New York Post. https://nypost.com/2020/08/24/beirut-faces-mental-health-crisis-after-blast/
Reuters Staff. (2020, July 17). Major Beirut medical center lays off hundreds as crisis bites. Reuters. https://www.reuters.com/article/us-lebanon-crisis-aub/major-beirut-medical-centre-lays-off-hundreds-as-crisis-bites-idUSKCN24I2GW
Schuster, K. (2020, August 28). Beirut’s deadly explosion created massive pollution – How bad is it? EcoWatch. https://www.ecowatch.com/beirut-explosion-pollution-2647369268.html?rebelltitem=3
Strategy&. (2020). (rep.). Beirut explosion impact assessment. PwC Network. Retrieved from https://www.strategyand.pwc.com/m1/en/beirut-explosion/beirut-explosion-impact-assessment.pdf
Tilsed, J., Borji, J., Hallal, A., Hoballah, J., Juvelekian, G., Safadi, B., … Zago, M. (2020, December 9). ESTES 13 webinar “Beirut Port blast – Lessons learned”. YouTube. https://www.youtube.com/watch?v=GmaV6uyQxlE
United Nations Audiovisual Library. (2020, October 23). WHO / Lebanon emergency medical teams [Video]. Unifeed. https://www.unmultimedia.org/tv/unifeed/asset/2575/2575125/?jwsource=cl
United Nations Office for the Coordination of Humanitarian Affairs. (2020). (rep.). Lebanon Flash Appeal. Retrieved from https://www.unocha.org/sites/unocha/files/Lebanon%20Flash%20Appeal%20FINAL%2014%20Aug%202020.pdf
World Bank (2020, December 1). Lebanon is in a deliberate depression with unprecedented consequences for its human capital, stability, and prosperity.
https://www.worldbank.org/en/news/press-release/2020/11/30/lebanon-is-in-a-deliberate-depression-with-unprecedented-consequences-for-its-human-capital-stability-and-prosperity
World Health Organization. (2020, August 17). WHO situation report – Lebanon blast – Issue 5 (11-14 August 2020) – Lebanon. ReliefWeb. https://reliefweb.int/report/lebanon/who-situation-report-lebanon-blast-issue-5-11-14-august-2020
World Health Organization. (2020, August 18). WHO Iran Update 13052019: Lebanon explosion. https://www.who.int/emergencies/who-lebanon-partners-update-18august2020.pdf?ua=1
World’s Capital Cities. (2020, September 21). Capital facts for Beirut, Lebanon. Retrieved December 13, 2020, from https://www.worldscapitalcities.com/capital-facts-for-beirut-lebanon/#:~:text=Population%20density%20within%20the%20Greater,residents%20at%20June%2030%2C%202020
The authors would like to thank Karen Mackey for her support with research logistics. This study received funding from the Department of Behavioral and Community Health at the University of Maryland, School of Public Health
The author(s) have no relevant financial disclosures or conflicts of interest.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()