MacEachron S and Watt P. An epidemic within a pandemic: the impact of COVID-19 on substance use in the United States. HPHR. 2021;48.
DOI:10.54111/0001/VV9
The year 2020, marked by social distancing, mask mandates, lockdowns, economic downfall, and death, will forever be remembered as the year COVID-19 spread across the world. In the U.S., states were left to set their own guidelines and regulations, with Michigan earning a reputation as one of the stricter states1 while other states declined to implement any lockdown measures at all. Efforts to slow the spread of the virus resulted in Michigan’s lockdown from March 23rd to June 1st and businesses did not begin reopening until June 8th1.2 Despite the importance of lockdowns in reducing the transmission of COVID-19, these public health mitigation efforts contributed to a new health crisis: social isolation. In an attempt to deal with these difficulties and life changes, many Americans turned to substance use.3 This is significant, as mental health and substance use behavior have been shown to worsen due to the stress and isolation brought on by the pandemic.
Consequences of COVID-19 have produced a multitude of catalysts for both individuals at risk for and with a history of substance abuse. The pandemic has actualized an incredibly different lifestyle, with many experiencing less human interaction and further isolation due to lost jobs and physical distancing measures. In total, 20.6 million Americans lost their jobs from March to May 2020 due to the economic recession caused by the pandemic, increasing the toll of economic stressors.4 Additionally, stressors still existed for those who kept their jobs. In-person employees were faced with risk of contracting the virus, while many remote employees dealt with isolation and caring for children simultaneously.5 Evidence shows that stressful working conditions can result in increased substance use due to a sense of isolation or poor work-life balance.6 In addition, COVID-19 has proven to be about six times more fatal than the flu, at a death rate of about 0.6%7 and nearly one fifth of Americans know someone who has died of COVID-198. The emotional toll of losing loved ones is significant and can evoke substance use.9 These circumstances are important to consider because stress and social isolation, which have been significantly exacerbated by the pandemic, have proven to be a risk factor for premature death, heart disease, stroke, dementia, and poor mental health.10
Nationally, both opioid and alcohol use have significantly grown over the course of the pandemic. Indeed, in 2018, 67,300 Americans died as a direct result of overdose11. In 2019, drug overdoses increased over 4% from 2018, with an age-adjusted rate of overdose deaths of 20.7 per 100,000 in 2018 and 21.6 per 100,000 in 2019.12 Despite overdose deaths already increasing prior to the pandemic, the latest numbers indicate an acceleration of overdose deaths greater than expected during the pandemic; the United States reached a disheartening milestone of the highest number of overdose deaths ever recorded in a 12-month period in May 2020 with over 81,000 Americans lost.13 Preliminary analyses of 2021 data indicate that overdose deaths increased in nearly every state during the first eight months of 2020.14 In addition, alcohol consumption has grown by 14% for men and 17% for women compared to last summer; this includes a 41% over baseline increase in heavy drinking for women.15 Therefore, on a national level, this has become an urgent issue.
Widespread increases in substance use across the United States have been reflected in individual states, including Michigan, Missouri, and Florida. More than 40 states have reported upturns in opioid overdose since the beginning of the pandemic3. Michigan has had similar outcomes. The EMS response in Michigan for opioid overdose from April to June of 2020 was up 26% from the same period in 201916. In addition, emergency department visits for opioid overdose increased by 2% over this period, while visits for other reasons decreased by 38%16. This increase was true for all demographics and regions, except for those aged 65 years and older.14,16 Changes in substance use and overdose did not seem to depend on the amount of restrictions a state placed on their population. For example, Missouri was ranked 12th out of all states, with states being ranked from the least to most restrictive.17 Despite Michigan being ranked the 31st state, Missouri saw a 29.0% increase in overdose, while Michigan saw a 22.6% increase.14,17 A more stark contrast with Michigan was Florida, which ranked 8th and had a 49.9% increase in overdose deaths1.14,17 Therefore, it appears that increases in substance use persisted regardless of state-level COVID-19 restrictions.
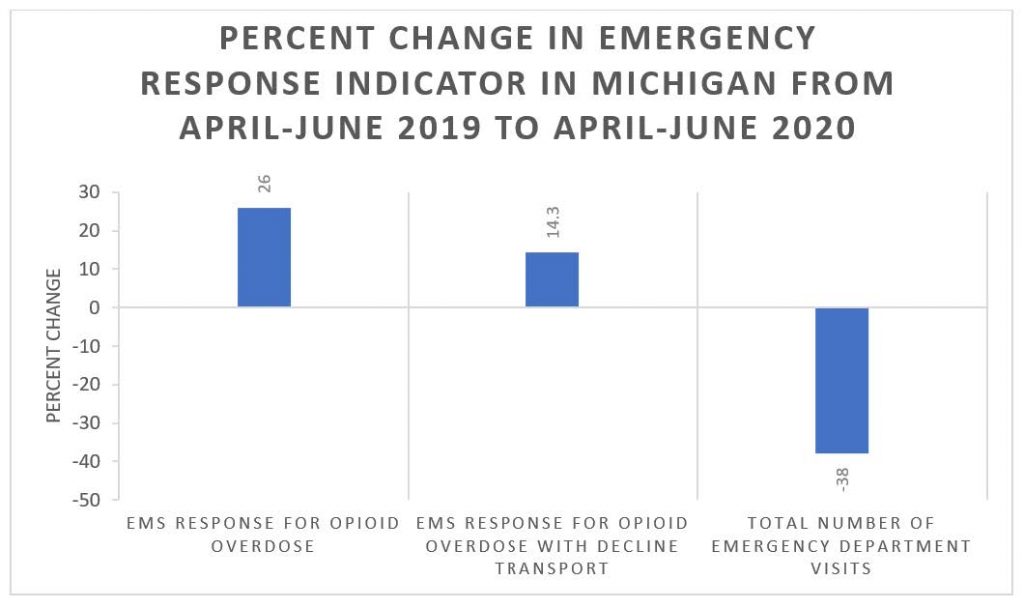
Table 1
Comparing emergency medical service (EMS) response for opioid overdose from spring of 2019 to spring of 2020– of which the latter included lockdowns and social distancing– shows an increase, both generally and with decline for transport.16 In contrast, the total number of emergency department visits decreased.16
The long-term impacts of substance abuse are devastating and long-lasting. Individuals in recovery are more likely to have difficulty obtaining a job18 and approximately 28% of individuals with substance use disorder have mental health challenges, such as anxiety and/or depression.19 Individuals who abuse substances also have an increased risk of chronic diseases20, strained relationships with friends and family.21,22 incarceration, and homelessness.23 On a larger scale, substance use and abuse costs society $820.5 billion every year due to crime, lost work productivity and health care.6 In order to mitigate these consequences, state and national leadership need to take action. As recommended by the American Medical Association, institutions should consider loosening restrictions on evaluation and prescribing requirements, removing barriers to medications to treat substance use disorders, and establishing harm reduction strategies.3 Leading experts in the opioid epidemic have suggested ways to mitigate the rising crisis from the pandemic, including removing stigma, ensuring telehealth access to care, and providing treatment for those with substance use disorder.23,24 Public health intervention is needed as an increasing number of American communities suffer the consequences of rises in substance use, even as the COVID-19 pandemic begins to slow.
Sierra MacEachron recently graduated from the University of Michigan School of Public Health with her Master of Public Health in Epidemiology and a certificate in social epidemiology. She is passionate about promoting health equity and is currently working as an epidemiologist at a local health department.
Payton Watt is a Master of Public Health student at the University of Michigan studying Epidemiology and Health Management & Policy. She is a 2021 David A. Winston Health Policy Scholar and is currently an administrative intern at UCHealth in Colorado. She is interested in social determinants of health, chronic disease, and health policy and administration.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()