Bowder A, Truche P, Buda A, Alkire B. Evaluating the macroeconomic burden of potentially averted surgical deaths under five. HPHR. 2021;34.
DOI:10.54111/0001/HH8
Increasing the worldwide surgical, anesthesia, and obstetric (SAO) workforce to 20-40 providers per 100,000 people could prevent anywhere from 273,000 to 600,000 deaths under age five annually. Utilizing VSL, we can calculate the value of welfare loss regions would face if we fail to prevent these deaths annually.
To estimate the total global economic welfare losses related to potential averted surgical deaths under age five, we first estimated country-specific values of statistical life, adjusting for the relationship between VSL (US and OECD) and income (income elasticity 1.0 and 1.5), and multiplied this by the averted pediatric deaths in each country that would be expected with an increase in the SAO workforce worldwide. We used GNI data from 2018 and estimates of under five deaths by Truche et al.
With a US VSL, elasticity of 1.5, and deaths averted by increasing the global SAO workforce to 40 per 100,000, we estimate 175 billion dollars in economic welfare losses could be prevented. This loss would affect low- and middle-income countries the most representing 2.04 to 4.48% of their GNI.
The loss of 600,000 children lives annually alone should inspire and motivate future policy, but the added potential economic welfare losses stress the importance of developing national policies aimed at providing safe, accessible, and affordable surgical care worldwide.
Recently Truche et al estimated that increasing the worldwide surgical, anesthesia, and obstetric (SAO) workforce to 20-40 providers per 100,000 people could prevent anywhere from 273,000 to 600,000 deaths under age five annually. Preventing these deaths would make great strides towards the 2030 goal of reducing under five mortality, while assessing their economic impact has the potential to guide future global surgery policy.
The concept of the value of a statistical life (VSL) is used by economists primarily in the context of benefit-cost analysis. The VSL is derived by assessing the amount individuals are willing to pay (or accept) to decrease (or increase) their risk of mortality by some small degree. Of note, it does not purport to reflect the actual value of an individual person’s life, which is infinite. Utilizing VSL we can calculate the value of welfare loss regions would face if we fail to increase the surgical workforce to 20-40 SAO per 100,000 people.
To estimate the total global economic welfare losses related to potential averted surgical deaths under age five, we first estimate country-specific VSLs, which requires adjusting for the relationship between VSL and income (the income elasticity, Appendix 1). We then multiply this by the averted pediatric deaths in each country that would be expected with an increase in the SAO workforce worldwide to 20-40 surgeons per 100,000 people (Truche et al, 2020).
Equation 1: VSLCountry = 2 x VSLUS x (IncomeCountry/IncomeUS)Income Elasticity (1 or 1.5)
Equation 2: VSLCountry = 2 x VSLOECD x (IncomeCountry/IncomeOECD) Income Elasticity (1 or 1.5)
Equation 3: VWLCountry = VSLCountry x Averted DeathsCountry
Few formal studies exist that estimate the VSL in low- and middle-income countries (LMICs), however there are methods for estimating VSL in a country where formal studies do not exist. We adjusted country-specific VSL’s for income based on current recommendations from Robinson et al (Hammitt & Robinson, 2011; Robinson et al, 2019). We assumed that the VSL of a child is twice that of an adult, similar to other authors in the field (Boardman et al, 2017). We used two base VSLs to estimate country-specific VSLs: the VSL used by the Department of Health and Human Services in the United States, and the VSL base estimate used by OECD (Equation 1 and Equation 2) (Boardman et al, 2017; Robinson et al, 2019). The value of the total economic welfare losses (VWL) as a result of under five mortality was then calculated (Equation 3), and that value was divided by a country’s GNI to present our results in the context of the size of a country’s economy. The reference estimates for VSL in this study were: U.S. VSL estimate – $9.3 million, U.S. GNI – $20.6 trillion, OECD VSL estimate – $3 million, and OECD GNI – $52.7 trillion (Robinson et al, 2019).
2018 GNI data (or the most recent year available) was obtained from the World Bank Open Database for 165 WHO member states (World Development Indicators, n.d.). The estimates of potential deaths averted for children under five were obtained from a model published by Truche et al (Truche et al, 2020).
Ethical approval was not required as the database accessed contains open-access data.
Using a US VSL, elasticity of 1.5, and deaths averted by increasing the global SAO workforce to 40 per 100,000 we estimate 175 billion dollars in economic welfare losses could be prevented (Figure 1). To provide a sense of scale estimates of welfare loss as a proportion of GNI (VWL/GNI) by world bank income classification are shown in Table 1. It appears LMICs would be the most affected if the SAO workforce is not increased worldwide. For sensitivity analysis we calculated a range of value of welfare loss accounting for income elasticity, US VSL and OECD VSL, as well calculations based on the number of under five averted deaths with 20 versus 40 SAO providers, this data is included in Table 1. We also include the value of welfare loss by country in Appendix 2.
These results highlight the significant economic burden avertable deaths of children under age five related to surgical disease will have worldwide: an increase in SAO providers to recommended numbers could potentially save 10.3 to 28.6 billion dollars (using the most conservative estimates) in lost economic welfare annually. We recognize that debate exists on the best method to calculate VSL for children. By including sensitivity analysis, and utilizing prior calculations of VSL for children, we report the estimates in our final result using conservative assumptions with regard to how VSL changes with income in an attempt to mitigate these concerns. The potential loss of 600,000 children lives annually alone should inspire and motivate future policy, but the added potential economic welfare losses demonstrated by this study add weight to the importance of developing national policies aimed at providing safe, accessible, and affordable surgical care worldwide.
This is one of the first studies of its kind attempting to estimate the macroeconomic burden of potentially avertable deaths under the age of five related to surgical disease. However, our results need to be interpreted in the context of several limitations including relying on modeled data. VSL calculations are derived from assessing the amount individuals are willing to pay to change their risk of mortality by a small degree, and it is likely that the linear assumption that is made to determine these values is too simplistic to represent a complex concept (Alkire et al, 2015). In addition, VSL refers to populations in aggregate, and may not take into account stark differences in social determinants of health and variations in access to care, nutrition, transportation, and exposure to violence across different groups within a population which may change an individual’s willingness to pay to avert death. Finally, due to the small number of VSL studies and a paucity of morbidity and mortality data in LMIC settings, our results are estimates that do incorporate variations in income through our calculations in order to account for this setting (Alkire et al, 2015). However, our study demonstrates that even with the most conservative estimates investing in the scaleup of the surgical workforce worldwide could have significant macroeconomic benefits, specifically related to surgically preventable deaths under the age five.
Table 1: All Averted Deaths Under Five by Income Group (VWL/GNI as percent)
LIC | LMIC | UMIC | |
VWL/GNIa (20 SAO) | 0.22% | 2.04% | 0.49% |
VWL/GNIa (40 SAO) | 0.43% | 4.48% | 0.59% |
VWL: value of the total economic welfare losses
E: elasticity constant
aThe data was calculated using a US VSL and an elasticity constant of 1.5.
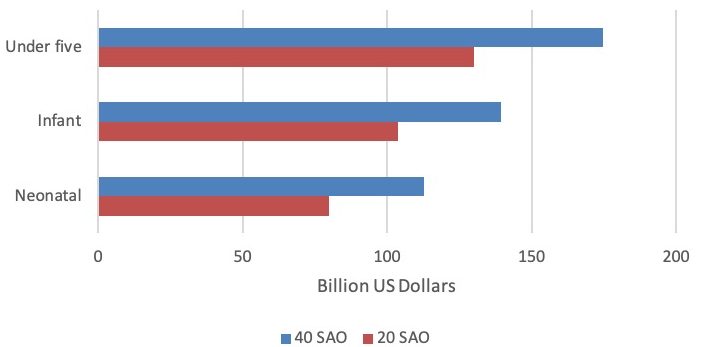
Title: VWL for All Averted Deaths by Age Group (Neonatal, Infant, Child) (in billions)
VWL: value of the total economic welfare losses
E: elasticity constant
*Of note, the value of welfare loss for the under five age group includes the values provided for both the infant and neonatal age groups.
Boardman, A. E., Greenberg, D. H., Vining, A. R., & Weimer, D. L. (2017). Cost-Benefit Analysis: Concepts and Practice. Cambridge University Press.
Hammitt, J. K., & Robinson, L. A. (2011). The Income Elasticity of the Value per Statistical Life: Transferring Estimates between High and Low Income Populations. Journal of Benefit-Cost Analysis, 2(1), 1–29.
Robinson, L. A., Hammitt, J. K., & O’Keeffe, L. (2019). Valuing Mortality Risk Reductions in Global Benefit-Cost Analysis. Journal of Benefit-Cost Analysis, 10(Suppl 1), 15–50.
Truche, P., Botelho, F., Bowder, A., Levis, A., & Mooney, D. P. (2020). Potentially Avertable Child Mortality Associated with Surgical Workforce Scale-Up in Low- and Middle-Income Countries: A Global Study. Journal of the American College of Surgeons, 231(4), S129.
World Development Indicators. (n.d.). Retrieved December 18, 2021, from https://databank.worldbank.org/source/world-development-indicators
Alkire, B. C., Shrime, M. G., Dare, A. J., Vincent, J. R., & Meara, J. G. (2015). Global economic consequences of selected surgical diseases: a modelling study. The Lancet. Global health, 3 Suppl 2(Suppl 2), S21–S27. https://doi.org/10.1016/S2214-109X(15)70088-4
Alexis N. Bowder, MD, MPH obtained her medical degree from the University of Nebraska Medical Center and is a general surgery resident at the Medical College of Wisconsin in Milwaukee. She has field experience in Haiti, Jamaica, Nepal, India, Honduras, and Peru. Her particular interests include strengthening surgical research capacity and improving access to pediatric surgical care in low and middle income countries.
Paul Truche, MD, MPH is a chief research fellow at Harvard Medical School’s Program in Global Surgery and Social Change. He is a general surgery resident at Rutgers Robert Wood Johnson Medical School and plans to specialize in pediatric surgery. His research interests include health system monitoring and modeling to guide support for access to safe, high quality, and affordable surgical care in all settings.
Alexandra M Buda, BS is a current medical student at the University of Rochester and research associate at the Program in Global Surgery and Social Change through Harvard Medical School.
Blake Alkire, MD is Assistant Professor of Otolaryngology at Harvard Medical, and with the Program in Global Surgery and Social Change, Harvard Medical School, in Boston, MA, USA.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()