Akhtar S. Interorganizational collaborations and improving surgical access to pediatric cardiac care in Pakistan: a non-governmental organization’s perspective. HPHR. 2021;34.
DOI:10.54111/0001/HH23
Infectious diseases, such as diarrhea and pneumonia, account for almost half the global burden of premature death in children in low-and-middle income countries (LMIC). The persistent global response has helped reduce this ratio substantially over time. This should redirect the call to action towards non-communicable diseases. Pediatric congenital heart disease (CHD) can be cited as one of the leading causes of avertible mortality in Pakistan. One of the main reasons is the inability of patient families to access timely surgical treatment. This can be attributed to (i) low prioritization of CHD management by the government (ii) low resources such as workforce, medical supplies and technology and (iii) inadequate financing options. Engaging international stakeholders towards CHD complex care in Pakistan presents challenges. To make surgery more accessible, domestic solutions provide more feasibility. This paper provides a commentary of an NGO’s perspective on integrating Interorganizational Collaborations (IOCs) into the existing CHD infrastructure in Pakistan as an innovative approach to tackling these challenges.
On 23 December 2020, Taiwan reported its first local COVID-19 transmission in more than eight months. Taiwan’s world-leading 253-day streak ended with a woman who was a close contact of a foreign pilot who travelled while infected. The pilot, an employee of a Taiwanese airline, is thought to have been infected during a flight to the United States (US) in November 2020. Despite Taiwan’s strict mandatory 14-day quarantine for most of its arrivals, pilots are only required to isolate for three days and are not tested if they are asymptomatic.[1] In this case and during the previous months, a robust track-and-trace program along with its proactive testing enabled Taiwanese authorities to effectively contain the infection with only a total of 942 confirmed cases equivalent to daily confirmed cases of 39 per million population as of 21 February 2021. Taiwan has achieved one of the lowest mortality burdens among high-income territories and achieved elimination by April 2020 without a lockdown. Its success in keeping the virus out has enabled the country to open its borders and return to relative normality in recent months.[2] This paper aims to discuss the key elements of success in Taiwan’s approach, highlighting lessons applicable in the time being and in the post-COVID-19 era.
The congenital heart disease (CHD) health system infrastructure in Pakistan faces a compounding problem of a high disease burden, low resources and debilitating financing options. Approximately 60,000 children are born with CHDs in Pakistan annually (Khokhar, Gova, Bangash, & Tahir, 2019). Around 25% of these children require surgical treatment within one year (UK, 2020). Without surgery, 60% of pediatric CHD patients cannot survive beyond the first few years of life (Khokhar, Gova, Bangash, & Tahir, 2019). Bringing the neonatal mortality rate (NMR) attributed to CHDs in Pakistan to 3.7% (Hassan, I., Haleem, A., & Bhutta, Z, 1997). Continued gross neglect to simplifying surgical access will inadvertently lead to an increase in these ratios. Which will worsen Pakistan’s population health status as neonatal and infant mortality rates (IMR) are already very high in the country (Organization, 2011).
CHD affiliated health resources are also scarce. There are only 3 pediatric intensive care units (PICU) for complex cardiac care in Pakistan (Khokhar, Gova, Bangash, & Tahir, 2019), 8 pediatric cardiac surgeons and 25 pediatric cardiologists nationwide (Khokhar, Gova, Bangash, & Tahir, 2019). In hospitals, an estimated 1600 patients have to wait for surgery with 2-3 children per bed (Pakistan, 2016). To address the CHD burden on the health system efficiently, approximately 22,000 CHD surgeries should be performed annually. Instead, roughly only 4,000 patients receive treatment (UK, 2020). Leading to an extensive backlog of patients in an already saturated health system. Many children, including those with simple CHDs, die while waiting for surgery.
Modes of financing and cost of surgical services also add limitations to access. In Pakistan, less than 7% of Gross Domestic Product (GDP) is allocated to health (Pakistan, 2016). Of this budget, a meagre 3% is directed towards tertiary hospitals in the public sector. Even though the CHD incidence rate in Pakistan is high, neighboring India reports a staggering incidence of around 200,000 per annum (Saxena, 2018). 5.4% of India’s GDP is focused towards the public health sector (Mondal, 2021). Despite this, the pediatric CHD surgical turnover in India is higher in contrast to Pakistan’s. The CHD surgical turnover in India is 85% more, at 27,000 surgeries per year. This is because extended government schemes, mostly at state level, cover about 40% of all surgeries for CHD patients (Saxena, 2018).
Where the overall health budget is already limited, there is hardly any financing left for the pediatric CHD sector in Pakistan. The cost of one corrective surgery is around $3-4,000 (Khalil, 2015). Often, multiple surgeries are also required for post-operative correction of residual CHDs. When compared to India and the US, however, Pakistan reports a lower average cost per CHD surgery (Pasquali et al., 2014). Despite this, a smaller number of CHD surgeries are performed in comparison. This reiterates the problem of limited access to surgical treatment in Pakistan. Moreover, around 29.5% of Pakistan’s population lives below the poverty line (Secretariat, 2018). Making the primary mode of finance for surgeries Out of Pocket Payments (OOPs). Healthcare expenditure as OOP in Pakistan is a staggering 98%. Positioning Pakistan among those countries with the highest share of OOPs relative to total health expenditure (EMRO, 2021). This has grave implications for financial risk protection for the population. Paired with a high poverty index, low resources and long waiting time, this makes surgical access extremely prohibitive for indigent patients.
The basis of the model is a nationwide, horizontal integration of a CHD based NGO with tertiary care hospitals offering pediatric cardiac treatment. This creates an IOC system that works through in-network referrals. Each IOC hospital is mutually responsible for providing all necessary resources for timely surgeries of patients through a Memorandum of Understanding (MoU). 15% discounts on all standard packages for CHD surgeries is levied as fee-for-service incentives for the network hospitals. The cost of disposables and consumables is also discounted at 15%. In cases of mortality, some IOC hospitals commit to forego all their fees and charges, including hospital and diagnostic services. Surgeons and all medical staff are reimbursed in full on a successful case and partially in the event of a mortality. IOC hospitals continue to receive an estimated 33% hospital service charge. This presents itself as a further incentive to stay in-network and, therefore, provide dependability of a sustained surgical resources.
Finally, a detailed bill is sent to the NGO at the time of discharge and has to be settled within 60 working days from the date of the invoice and at a maximum of $32,000 outstanding. This credit-reimbursement payment system allows patients to receive surgical treatment at the nearest appointment instead of waiting for surgery while arranging finances. Thus, through referrals, the NGO’s partnerships with hospitals allows (i) distribution of patient volume across the IOC hospitals (ii) an increase in patient turnover because of an alternative revenue source and (iii) overcoming low resources, such as surgical equipment, medicines, and healthcare professionals, through utilization of resources collated via the network. This collaboration presents the added advantage of patient data collection and recording at a single CHD registry maintained by the NGO. Which will facilitate research initiatives, quality improvement and implementation of evidence-based surgical practices. This is imperative because apart from, Bushra, Muneer, & Mehnaz (2013), there is currently no published data on CHD surgical outcomes in Pakistan. Finally, additional funding is sourced by forming IOCs between both national and international corporate social responsibility sectors of other organizations.
IOCs with other health-based NGOs helps with subsidizing surgeries and increasing patient turn over by (i) adding external funding to the CHD network through donations and by (iii) additional media for increasing referrals. 50% division of expenses between both parties is mandated. Partnerships with international NGOs also offer more resources to help build sustainable pediatric cardiac programs in LMICS. In countries like Pakistan, to improve access to surgery, it is also important to overcome the stigma of seeking treatment and to create an awareness of available treatment options. Global collaborations assist in research-based awareness and advocacy of CHDs. These partnerships also extend towards quality improvement collaboratives and for measuring surgical outcomes using global standard sets.
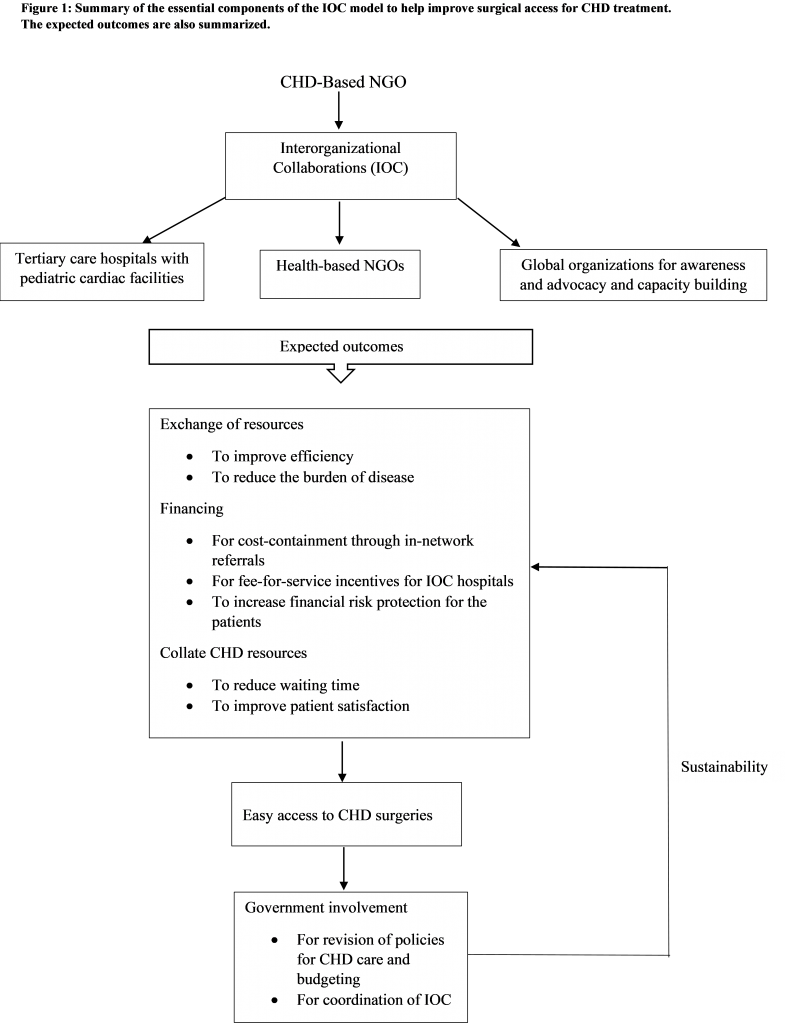
Finally, to tackle a deficient health workforce, IOCs with national and international tertiary care hospitals and NGOs provide a platform for capacity building. These IOCs help train junior health professionals in innovative CHD management techniques through medical missions or workshops. The objective is to increase resilience and skill amongst the health professionals to tackle low resources in the country. This also allows training of health professionals in a short period of time. Figure 1 summarizes an NGO’s perspective of an IOC model incorporated into the CHD infrastructure in Pakistan.
The illustrated model has shown potential in different contexts. For improving health service delivery in other health sectors, Hall et al. (2019) reports its effectiveness in Timor-Leste. The systematic review concluded an improvement in the mental health status of the population because of IOCs between non-clinical and mental health services. In the context of public-private partnerships (PPP), the Poor Patients Relief Program in Nepal provides free health services to the indigenous population. Service delivery is through government engagement with NGOs and private hospitals/clinics (Saxena,2018). The Narayana Health Program in India is an extensive partnership program between multidisciplinary hospitals. This partnership helps provide affordable treatment, covering 30 medical specialties (Saxena, 2018). In Pakistan, IOC in a PPP context has demonstrated success in primary health care. The District Rahim Yar Khan Project incorporates an IOC between Basic Health Units (BHU) and the Punjab Rural Support Program, an NGO (Ejaz, Shaikh, & Rizvi, 2011). In the CHD sector, however, a PPP based IOC presents challenges. Of the 5 hospitals providing CHD surgical services, only 2 are in the private sector. Additionally, all these centers are present in an urban setting. Promoting IOCs between health NGOs would have to be prioritized for CHD surgical outcome improvement, initially.
Utilizing the IOC Model for Sustaining Surgical Access Replicability of this framework offers potential for improving the efficiency and quality of complex care through the CHD non-profit sector. Improvement in access to surgery can subsequently provide a directive for the revision of existing CHD healthcare policies and budgeting by the government. Policy change will allow more efficient coordination of CHD IOC programs in the country. Implementation of The Global Initiative for Emergency and Essential Surgery Care (GIEESC) by the World Health Organization (WHO) can also help the government coordinate the model. The GIEESC is a global initiative that helps improve access to surgical treatment through IOCs and referrals in LMICs. The most frequently used assessment tool by this program is the WHO GIEESC SAT. It covers infrastructure, human resources, procedures, equipment and supplies (Bickler & Spiegel, 2009). The four components central to this IOC model (Figure 1).
The existing CHD health sector in Pakistan is composed of a limited tertiary care infrastructure, resources and skilled professionals. Healthcare facilities offer either a combination of free adult and pediatric cardiac/CHD surgeries or pediatric general surgery. Keeping the limitation of resources in mind, the idea is to build on this existing CHD platform to increase the efficiency of this sector. Due to the scale of the problem, there is a need for enhanced alliances in the CHD/health-based social sector in Pakistan. Replicability of the IOC framework by other CHD/health-based organizations in the country can help facilitate surgical access for patients. Relying on national resources provide cost-effectiveness and time sensitivity. A timely improvement in CHD surgical outcomes can help improve the NMR and IMR. Encouraging a possible government stake towards the CHD sector. Government inclusion will offer scalability and sustainability to the CHD infrastructure. It will also allow for the retention of and acquisition of diverse and global stakeholders. In conclusion, IOCs for CHD healthcare propose a holistic approach for facilitating access to CHD surgeries in Pakistan.
Dr. Samaa Akhtar, MD, MSc (London) is an experienced physician-scientist who is an ardent advocate of improving patient care and health systems through clinical and translational research. Following completion of her Bachelor’s in Medicine and Surgery from NUST (Pakistan), she went on to complete her Master’s in Health Policy, with a concentration in public health, from City, University of London (United Kingdom). Additionally, Dr. Akhtar has completed a certification in Health System Strengthening from John’s Hopkins Bloomberg School of Public Health (United States). She is also certified in the International Conference on Harmonization-Good Clinical Practice (ICH-GCP). Dr. Akhtar is a member of the European Society of Cardiology and The Global Health Network. She also volunteers as contributing researcher in the Oli Healthcare Magazine Organization (OHMO) and as a peer-reviewer for The Cureus Journal of Medical Science. Her research has been published in coveted journals such as The Harvard Public Health Review (HPHR) and the Journal of Infection Control and Hospital Epidemiology (ICHE), among others. Dr. Akhtar is currently working as a Senior Research Fellow and Chief Advocacy Liaison in pediatric cardiology, with a concentration in congenital heart diseases, at the Children’s Heart Hospital and Research Institute (Pakistan). Her research areas of interest include non-communicable diseases, global health, global surgery, and artificial intelligence in healthcare.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()