Carpenter C, Makhubu K, Moche L. An invisible public health crisis: the forced normalization of intersex people. HPHR. 2021; 30.
DOI:10.54111/0001/DD14
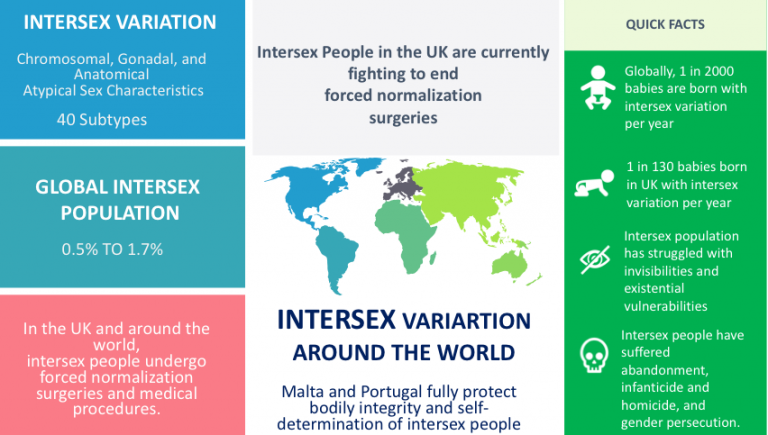
Despite the burgeoning knowledge about health issues for people within the LGBTQ+ spectrum, many public health practitioners remain intellectually oblivious to the existence of the intersex community. However, within the shadows of the battle for gay marriage and transgender rights has been a quiet, albeit global intersex movement. Although countries such as Portugal and Malta have given full protection to the bodily integrity and self-determination of intersex people, other countries have lagged behind. Whilst the United Kingdom (UK) does have some anti-discrimination laws for intersex people, it presently classifies and treats intersex people as second-class citizens. Ultimately, the UK lacks laws protecting the physical integrity and bodily autonomy of intersex bodies. This paper illuminates the public health and human rights crises of intersex people in the United Kingdom using a systems-based analysis. It also highlights legislative actions undertaken, as well as recommendations for future research, education, and public health policy for intersex people.
Since 2006, intersex variation—in which the development of chromosomal, gonadal, or anatomical sex is atypical – has been characterized as Differences of Sex Development.7,9 However, intersex bodies existed since time immemorial.22 Intersexuality is hypothesized to occur during a non-normative process of sexual development and differentiation within the womb.17-20, 25-26 However, being intersex is not equivalent to being transgender or transsexual; nor is intersex variation so rare as to be easily forgotten.
Estimates of intersex variation range around 0.5% to 1.7% of the global population.35 Essentially, 1 in 2,000 babies are born with ambiguously designed sexual anatomy.2 As of 2017, the British Charity for DSD Families estimates that around 130 babies are born in the UK each year and necessitate investigation for sexual assignment.32 Spanning along the spectrum of genetic, chromosomal, and hormonal difference, at least 40 intersex variations have been acknowledged.29 However, considerable anecdotal evidence suggests that many intersex variations are subtler, manifesting later in life.38 Thus, the initial estimate of 1.7% of the global population may be grossly underestimated.
Intersex variations include graduations of genital ambiguity—such as micro-penis, clitoromegaly, partial labial fusion, delayed or absent puberty, hypospadias, and labial or inguinal masses.17-20, 25-26
After the 1950s, John Money’s medical models of “concealment care” and “optimum gender of rearing system” were widely adopted throughout the global medical community.22 Both intersex advocacy and medical groups point to these models as the initial medicalization of intersex people, and the springboard for normalization surgeries.9,12 According to the Intersex Society of America, intersex surgeries around the world have been conducted by inferior standards for which general anatomy is arbitrarily and illogically determined and designed.22 The rationale for normalization surgeries varies not only from country to country, but also from region to region, hospital to hospital, and doctor to doctor.12 Globally, the standard of care for intersex patients remain uneven, inadequate, and piecemeal in design.16
Many human rights organizations have staunchly lambasted the medical profession for stripping intersex people of both social context and autonomy vis-à-vis the medicalization process. They have further objected to the clinical aura of indifference, paternalism, and ethnocentric cultural myopia toward intersex people that exists in many countries.38
The intersex population has often struggled with invisibilities and existential vulnerabilities. From antiquity to even the present day, people with intersex variation have suffered abandonment, neglect, attempted murder, infanticide and homicide, and gender persecution.6,31 Undergirding the perpetuation of violence against intersex people has been a bulwark of cultural, religious, traditional, and medical beliefs and practices in regions throughout the globe.3
To the medical community in the UK and around the world, the correction of ambiguous intersex traits (e.g., when genitalia does not appear definitively male or female) into a singular genital entity is referred to as “normalizing surgery”.7,9
Also referred to as “feminizing surgery”, “masculinizing surgery”, “genital sexing”, “surgical sexing”, and “genital re-shaping” surgery, normalizing surgery of intersex people became popular and institutionalized in the early 20th century.37 Surgeries include procedures like vaginoplasty, clitoral reduction, and gonadectomies.8,13 These surgeries are typically conducted on babies under 24 months of age.8 Forced normalization of intersex people can also occur via hormonal alteration.29 Of the most extreme, according to the UK Human Fertilization and Embryology Authority, forced normalization entails genetic pre-selection and termination of intersex traits that are deemed undesirable, such as Klinefelter’s syndrome, 5-alpha reductase deficiency, and androgen insensitivity syndrome.38
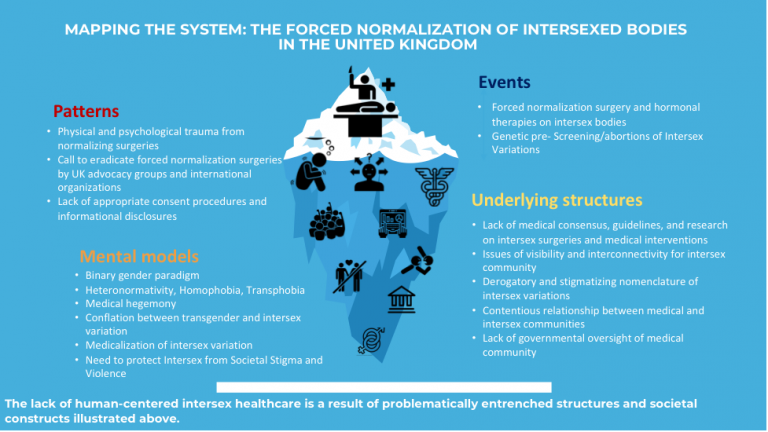
But how has the system of forced normalization of intersex bodies persisted? Below, we will discuss the multidimensional nature of this crisis, ranging from the lack of appropriate disclosure from medical personnel to patients and their families; lack of medical consensus, research, and guidelines; persisting derogatory language and minimizing attitudes; to the heteronormative, homophobic, and transphobic ideologies surrounding people with intersex variation.
Parents of intersex children are often given partial and pressurized information about the ‘urgent need’ for normalization surgeries and hormonal interventions.4,10 Some parents and intersex people even assert that the medical field outright lied to them about what surgeries they signed up for.13 Within the past year and a half, the UK intersex Association has launched a campaign against the widespread clinical practice of withholding information from intersex people regarding medical interventions and their physical and psychological implications.33
The absence of medical consensus and guidelines surrounding the practice of normalization surgeries is a linchpin to the problem.23 A clinical consensus on normalization surgery in the UK –specifically regarding surgical timing, necessity, type of surgical intervention, and surgical criteria – is non-existent. Within the past year, despite mounting criticisms, the National Health System expressed enthusiasm and approval of normalizing surgeries on intersex bodies.4
In addition, parents and intersex people avow the lack of full access to medical records.21-27 Within the UK, the medical records have been lost, disregarded, potentially destroyed, or kept hidden from intersex people.4 Coupled with the sweeping dearth of longitudinal studies and clinical trials regarding consequences of normalization surgeries on a national and global scale, evidence-based medicine regarding intersex people is minimal.7 Such scarcity of knowledge—and national commitments and international collaborations—reinforce the status quo of normalizing surgeries on intersex bodies.9,29
These Informational deficiencies further contribute to a sense of invisibility, as well as personal and communal invalidation. The difficulties in establishing a larger connected intersex community in the UK are consequently magnified.24
According to many intersex rights organizations, pejorative and stigmatizing language from doctors promotes normalization surgeries.11 Until the early 20th century, intersex people were offensively referred to as hermaphrodites.7 In 2005, a global and clinical consensus meeting on intersex bodies—which included two people from the intersex community and no ethicists or social scientists—cast intersex people under the umbrella term of Disorders of Sex Development, or DSD.7 However, the UKIA unequivocally expressed its strong disapproval and opposition to the DSD terminology. They promulgated that the term perpetuates the pathologization and stigmatization of intersex people within society, and reinforces support for normalization surgeries.38 Despite the objections of the global intersex community to current DSD terminology, there’s been no attempt to change these terms in the UK. In fact, objections have often met with resistance, cavalier attitudes, defensive posturing and disbelief from the medical community.38 Thus, the language battle highlights the contentious relationship and fragmentary discourse between the intersex and medical communities.11
In early 2019, despite the zeitgeist against intersex surgeries, the British government claimed it was unaware of the numbers of normalization surgeries in the country. Similarly, the British Department of Health, NHS England, and NHS digital all asseverated that they did not collate information on normalizing surgeries for intersex patients.4
Like most governments, the British government grants UK physicians carte blanche to implement medical interventions and conduct surgeries on all patients, including intersex people.4 Based on historical precedent and discomfort with breaking this precedent, there appears to be no governmental oversight of, or legislative action against, the medical profession, as medicine is universally regarded as a self-regulating, self-correcting, and inherently ethical Institution.31
The desire to preserve heteronormativity and the binary gender paradigm of male and female also reinforces the existence of gender-reshaping surgeries.34,37 Intersex researchers have noted parental homophobic or transphobic desires to keep their children from becoming “gay”, “queer, “gender confused”, or “gender-non-conforming”.22 Common clinical goals of normalizing surgery have been to make “real women” and “real men” who are capable of heterosexual and penetrative intercourse.12,16
Medical practitioners and patients have also cited a keen desire to sex-surgerize their intersex children to obviate societal bullying and social stigma they may experience.16 Intersex life is believed to be difficult if atypical genitals remain unchanged.13 The need to protect “social normalcy” has often been conflated with “medical necessity”.28
In 2001, however, the UK’s Journal of the Royal Society of Medicine significantly interrogated “normalizing” intersex practices due to prolific claims of irreparable harm incited by the normalization surgeries.8 It became abundantly clear that both a public health emergency and human rights crisis had been occurring for decades. To the intersex and global communities, normalization surgery, hormonal therapy, and genetic screen-outs of intersex variability are tantamount to infant genital mutilation, castration, and outright genocide.1,9
A cascade of anecdotal reports consequently revealed the multi-layered consequences of normalizing surgery. Several UK studies in the early 2000s demonstrated that 28% to 46% of patients reported unsatisfactory or poor cosmetic results from normalizing surgery.9 Reports published in the early 1990s reveal that normalizing surgery result in loss of sexual sensation in 20% to 50% of cases.11,38 On a physical basis, intersex people who had undergone normalizing surgery were more likely to lament permanent infertility, obligatory lifelong hormonal replacement and revisional surgeries, post-operative scarring, torn genital tissue, loss of bodily integrity, pain, incontinence, and loss of sexual arousal and pleasure.3,7,21 Psychologically, intersex people universally experienced more gender dysphoria, feelings of being assigned to the wrong gender, substance abuse, shame, confusion, suicidality, anxiety, trauma, and depression.4,15,38 Reports from secondary research reveal that due to the normalization surgeries and procedures, many intersex people frequently distrust health professionals and find healthcare interactions traumatic, sometimes to the point of eschewing any medical involvement– all of which contributes to poorly detected and ill-documented health disparities between intersex people and non-intersex people.4,38
Resultantly, within the past 20 years, there has been a movement to review all aspects of intersex normalization procedures, including diagnostic techniques, timing and nature of surgical and medical treatments, and consent processes.9,38 A clarion call—to end medicalization of intersex bodies, superfluous and unscrupulous normalization surgeries, hormone therapies targeting individuals with intersex variation—has echoed around the world. A litany of international human rights bodies have deplored normalization procedures as acts of cruelty and violations of human rights; they have called for intersex individuals to have freedom from torture and experimentation; right to health; right to autonomy and dignity; right to privacy; and right to bodily integrity.7,38 International bodies opposing normalization surgeries on intersex bodies include organizations like the UN Human Rights Council; UN Committee on Rights of Persons with Disabilities; UN Committee Against Torture; Intersex Society of North America; Swiss National Advisory Commission on Bioethics; Council of Europe; World Health Organization; UN Office of the High Commissioner for Human Rights; and Open Society Foundations. The UN committee has even published recommendations for the provision of full, free, and, informed consent for intersex people and their parents and guardians.4
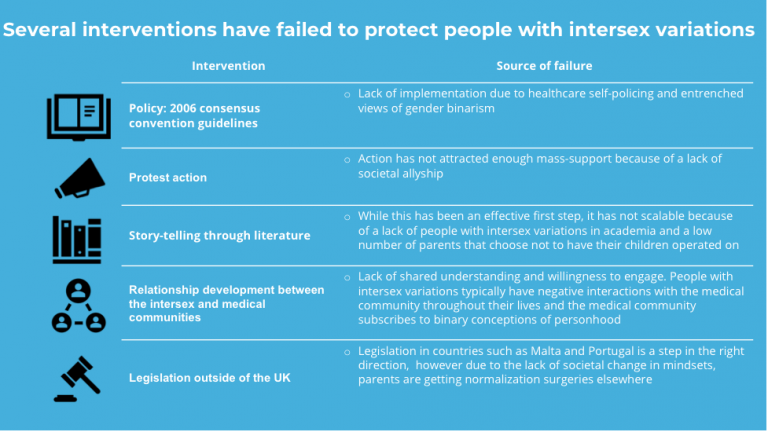
In 2015, Malta became the first country to outlaw non-consensual and medically unnecessary interventions on intersex bodies. While this legislation is ground-breaking, the law nonetheless “puts the impetus on the child to refuse these surgeries”. This implies that procedures can still happen. It does little to diminish the problematic perspectives against intersex traits and intersex people needing to be fixed.14 These changes in legislation without wholesale societal change has resulted in some Maltese parents getting the surgeries performed in different countries and even through domestic loopholes.5
In California, a legislative proposal to ban cosmetic surgeries on intersex bodies in 2019 failed primarily due to opposition from medical bodies that cited a rigid “one size fits all” solution as problematic.10 Even though the bill had widespread support from several civil society organisations and stakeholders including the Lesbian and Gay Medical Association, lawmakers submitted to the California Medical Associations opposition.10 Legislative change in the UK has been met with similar vociferation and sabotage. Medical hegemony and embedded societal gender constructs have made the eradication of normalization surgeries a Sisyphean task.
In an effort to raise awareness about intersex non-consensual surgeries, some intersex activist groups have employed protest action as a tool to pressure the medical community, lawmakers and DSD parents’ groups to change surgical and hormonal normalizing practices. The protests have not typically been mass-movements due to the fragmented nature of intersex variations and comparatively low allyship relative to the gay/lesbian/bisexual rights movement. It is impossible to quantify the impact that these protests have had. However, there is minimal evidence that protestation has ignited systemic change to protect children born with intersex variations.
Building a bridge between the intersex community and the medical community has had significant challenges. A lack of shared understanding and un-willingness to engage on both sides of the aisle has often led to gridlock. Members of the intersex community cite traumas resulting from the oppressive nature of lifelong medical interactions, whilst the medical community maintains its beneficence to help intersex individuals fit into society.30
There is a famous and oft-quoted phrase given to film students that says, ‘If we don’t exist in culture, then we don’t exist.” Similarly, creating space and visibility for intersex people is needed across the swathe of society – from arts and culture, to media to medicine, to law and public health research. Visibility and representation of the intersex community are poignant tools, not only for advocacy, but for the recognition and validation of their existence.
Akin to other liberation movements – like LGBTQ –attaining visibility for the intersex community will eventually translate into political justice, then legislative action, and finally the restoration of human rights.
We have seen the transformative and empowering force of research in feminism and the women’s rights movements through the works of Kimberley Crenshaw and Gloria Steinem, and more recently in the transgender equality movement. Recognizing intersex bodies and experiences within public health research is a similar legitimizing force for change. Public health literature and knowledge are important tools for advocating for the right to be of intersex people. How intersex people are understood in public health literature informs how they are treated in the medical, legal, and public space.
Other proposed solutions include funding more research on intersex experiences, as well as funding intersex people to study and pursue postgraduate degrees. Projects such as the Intersex: New Interdisciplinary Approaches (INIA) – which fund early-stage researchers from the European Union to pursue doctorates relating to the physical, psychological, and emotional health of intersex people—are important projects that need to be amplified and replicated at scale.36
Furthermore, there needs to be a simultaneous demand for updated and evidence-based clinical research on the best medical, surgical, and psychological care for intersex people. Ample research and education will help to pave the way for much needed policy around the human and health rights of intersex people.
The public health and human rights emergencies against intersex people must be made visible and writ large. Just as the public health practitioner and social justice advocate seek to eradicate racism, sexism, ableism, homophobia and transphobia as determinants of health, so should they strive to eliminate the forced normalization of intersex bodies and its devastating impacts on the physical, psychological, and emotional health of intersex people.
Dr. Carpenter is a physician, entrepreneur, educator, and social justice advocate. She is currently the Co-Editor-in-Chief of the Harvard Public Health Review.
Khaya Makhubu, MBA is a graduate of Oxford University.
Lee Moche, MBA, MS is a graduate of Oxford University.
HPHR.org was designed by ComputerAlly.com.
Visit HPHR’s publisher, the Boston Congress of Public Health (BCPH).
Email communications@bcph.org for more information.

Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of HPHR Journal.![]()